A complete blood count means counting the number of cells in a venous blood sample. Capillary blood is not a recommended testing medium for cell counting, but hemogram testing is often performed from a capillary blood sample in intensive care units.
Determination of the leukocyte formula, study of the average size of erythrocytes, platelets, determination of the number of erythrocyte precursors (reticulocytes) and the degree of their maturity, assessment of the erythrocyte sedimentation rate, etc., all this is included in the concept of “clinical blood test”.
A clinical blood test is performed as the first screening test when the patient complains of malaise. An abbreviated clinical blood test, the so-called “troika”, can be performed - counting the number of red blood cells, white blood cells and determining the erythrocyte sedimentation rate (ESR). An abbreviated clinical blood test is not very informative, because can characterize only pronounced pathological processes.
It is more advisable to perform a detailed hemogram from the same volume of blood sample: counting the number of red blood cells with an assessment of their average size (MCV), counting the total number of leukocytes and assessing the leukocyte formula (counting neutrophils, basophils, eosinophils, monocytes, lymphocytes), counting the number of platelets and assessing average platelet size (MPV), reticulocytes and their average size (MRV), reticulocyte maturity (IRF).
Numerous cell characteristics can now be obtained automatically within 3-5 minutes after blood collection. Based on a detailed study of the hemogram, not only a conclusion can be made about the presence of an inflammatory reaction, anemia, but also the nature of other pathological processes, possible previous or ongoing blood loss, deficiency of not only iron, but also vitamin B12 and folic acid.
Research method
The research method depends on the required parameters of the hemogram.
In manual mode, part of a blood sample (3–5 ml) is taken into a capillary to determine ESR, part of the blood sample is used to determine hemoglobin, a drop of blood is used to prepare a smear and further calculate the leukocyte formula. A separate amount of blood is required to prepare a smear and count platelets, and part of the blood sample is needed to study the number of red blood cells and, separately, reticulocytes. In manual mode, if staining and visual assessment of the smear are necessary, the result of a detailed hemogram of a patient in a multi-bed hospital can be obtained at the end of the working day or later.
In automated cell counting and evaluation of different populations, 150 to 300 μl of blood and 100 μl are required for ESR determination. Automatic testing is based on the impedance method of Coulter (1956), which is based on the principle of closing an electrical circuit with each cell successively passing through the sampler aperture. Subsequently, the automated counting method received a number of improvements; in modern analyzers, each cell is assessed according to several parameters: conductivity, light scattering, size, the presence of CD markers on the surface, and, accordingly, membership in different populations. The number of parameters is determined by the device model.
Automatic testing allows you to identify pathological samples that must be visually reviewed by a laboratory diagnostic specialist. Visual control of the hemogram involves preparing a blood smear or slide, which can be made from a drop of blood from an already taken sample, both manually and automatically. Automated blood smear preparation is preferable because There is a uniform distribution of the blood drop and standardized staining. Visual microscopy of the smear is carried out in five fields of view.
An automatic blood test takes 3–5 minutes, unless additional smear preparation and ESR testing are required.
When are skin tests prescribed?
Normally, the skin is evenly colored, moderately moist, and smooth. If any indicator changes, the changes bring obvious discomfort, the symptoms do not go away for a long time, you need to consult a doctor.
The skin is heterogeneous, and diseases affect its different layers: psoriasis and scabies - the epidermis, furunculosis - the dermis, cellulite - subcutaneous fat, etc. The first stage of any study is an examination and interview of the person, then based on primary external signs and information received The doctor decides what tests the patient needs to undergo to diagnose the disease.
An oral interview reveals the duration of the condition, the reasons - according to the patient, regularity (whether this happened before or for the first time), symptoms of the general condition, the presence of chronic diseases and diseases in relatives, colleagues, dietary features, living and working conditions, etc.
The specialist does a visual examination and, if necessary, prescribes tests:
- for various rashes in the natural folds of the skin, on the scalp, neck, face;
- with small whitish scales in the area of the nasolabial triangle, on the scalp, on the back, under the armpits, and in other places;
- with itching, burning;
- when plaques covered with scales appear, usually on the bends of the knees and elbows, in the areas of joints, on the palms, soles, and on the scalp;
- for bruising, swelling, ulcers;
- when papillomas appear;
- when spots of unknown origin are detected;
- for acne, pimples and other skin abnormalities;
- for some nonspecific symptoms.
Types of diagnosis of skin diseases:
General blood analysis:
- the presence/absence of an inflammatory process is determined by leukocytes and the leukocyte formula;
- according to erythrocytes, hemoglobin - leukemia, the presence of internal bleeding;
- for basophils and eosinophils - the presence/absence/strength of the allergic process.
The blood of a healthy person contains no more than 5% eosinophils. An increase in their proportion raises suspicion of an allergy. However, a high number of eosinophils is also characteristic of parasite infestation, which is why additional tests are required.
General urine analysis
Allows you to judge the presence/absence of an inflammatory process, determine whether diseases of the kidneys and other related organs are present.
Blood biochemistry
With the help of this analysis, one judges the metabolic processes in the body and obtains the most complete, systemic picture of its work.
Stool analysis
Using this analysis, parasites are identified that can cause an allergic reaction and inflammatory processes of the skin.
Immunogram
Using an immunogram, a preliminary diagnosis is confirmed. During the study, the blood is tested for immunoglobulins: if they are elevated, the disease develops.
Microscopy of scrapings
Scrapings are performed if scabies and mycotic (fungal) infections are suspected. For analysis, scales from the lesion and suspicious passages are used, which are placed on a glass slide and examined.
Epicutaneous and intracutaneous skin tests for allergic conditions
In some clinical situations, children and adults need to undergo an allergy examination, for example, patients with allergic rhinitis, bronchial asthma, atopic dermatitis, food allergies, reactions to drugs, etc.
With the epicutaneous method, the allergen is applied to the skin to identify the irritant in cases with a delayed hypersensitive response to the contact allergen. Intracutaneous (intradermal, intradermal) methods are used to detect an immediate hypersensitive response to a drug, bee venom and some other irritants. Intradermal tests are highly accurate. however, their disadvantage is a large number of false positive results.
Mycological, bacteriological, virological, serological tests for dermatoses caused by microorganisms
To identify microorganisms that cause diseases, use:
- scrapings of scales, nails, hair, which are specially processed and examined under a microscope - this is how pathogenic fungi are determined;
- discharge from the urethra, smear - to determine gonococci and other pathogens of STDs;
- smears-imprints on Tzanck cells from surfaces affected by erosion - to determine acantholytic pemphigus;
- skin scrapings - to identify scabies mites;
- tissue juice collected from the bottom of chancres - to determine pale treponema;
- cultural studies (cultures of pathological biomaterial) - to determine the causative agent of pyoderma, mycoses (including latent forms), STDs and carriage of deomatophytes.
Immunofluorescence tests for autoimmune diseases
Autoimmune skin diseases include blistering dermatoses - Dühring's dermatitis herpetiformis, pemphigus (true and all its varieties), pemphigoids.
These diseases are based on the body’s immune response aimed at intercellular contacts of the skin. Thus, pemphigus vulgaris is characterized by the appearance of antibodies to desmosomes, pemphigoid - antibodies to hemidesmosomes.
The developed disease is well diagnosed using serological tests - antibodies are detected in approximately 80%. But in the initial forms and damage to the mucous membranes, there are no antibodies in the blood, so direct and indirect immunofluorescence examination is used.
Direct immunofluorescence detects IgG and complement on cryostat skin sections. Indirect immunofluorescence reveals high titers of Ig G to desmosomes in the blood and fluid contents of the blisters - the higher the titers, the more severe the course of the disease.
Angiographic studies for vascular disorders
Vascular skin disorders - angiomas - include densely located blood and lymphatic vessels. Angiomas are located on and under the skin, changing its color to red and with a clear purple tint.
There are:
- Hemangiomas are pathological clusters of tumors from blood vessels, colored red or purple. Particularly common are childhood hemangiomas, which in 2/3 of children disappear by about 7 years, but leave “colored” marks or scars on the skin;
- flaming nevi - pink, red, purple flattened spots, by their nature - congenital defects of blood vessels;
- lymphangiomas - tubercles of different sizes on the skin formed by a cluster of lymphatic vessels;
- pyogenic granulomas - raised, fleshy, red, red-brown formations, moist or crusty, which are formed by rapidly growing capillaries and swelling of the adjacent tissue;
- Spider angiomas are bright red spots with a central blood vessel and capillaries extending from it in the form of spider legs.
If the skin damage is only cosmetic, your doctor will advise you on how to get rid of it. But sometimes angiographic studies are required - contrast studies of blood vessels using X-rays, CT, MRI, etc.
Histological examination
Histological examinations of the skin confirm or exclude a preliminary diagnosis and serve to determine the stage of the disease and the extent of the tumor. All this is necessary for correct diagnosis, prognosis and effective treatment.
For biopsy, a typical element is selected, preferably a fresh primary one. If the rashes are widespread, then the biomaterial is taken from such a focus, the removal of which will cause minimal cosmetic and functional defects.
The biopsy is performed under local anesthesia, using a scalpel or methods of puncture biopsy and electrosurgery.
Allergy tests
To determine the allergen, experts use different tests:
- prick tests (applying drops with an allergen to the skin, then piercing the drop with a prick lancet) - to identify sensitization to household, epidermal, pollen, medicinal, fungal and other allergens;
- scarification (scratches with special lancets containing allergens in cases where a skin prick test is not possible) - have high specificity. however, they often give a false positive result;
- application or patch tests (the allergen is applied to a patch that is glued to the back or shoulder) - to determine contact and atopic dermatitis.
Skin tests are assessed after 20 minutes, 6 hours or 24-48 hours, depending on the allergen. The test result may be negative, weakly positive, positive, or equivocal.
Additional Research
Serological (study of antibodies and antigens in blood serum)
With high sensitivity to a certain allergen in the blood, the content of IgE class antibodies increases, which in the normal state constitute approximately ~0.001% of all immunoglobulins. To identify the irritant, allergen-specific antibodies are determined.
Blood serum testing begins with determining the total level of immunoglobulin E (IgE). However, in approximately 30% of people susceptible to allergies, total immunoglobulin is normal, and increased levels can also be observed during helminth infestation and some other diseases.
Then a specific irritant is identified by determining specific IgG antibodies, for example, to food products, pollen, etc.
Microscopic (examination of a smear under a microscope)
Cytological examination is carried out for the purpose of morphological assessment of cellular composition, changes in cells (nucleus, cytoplasm, their ratio). Based on the data obtained, preliminary diagnoses of benign, malignant tumors, and other non-tumor lesions are made.
Pathomorphological (biopsy)
A skin biopsy is performed for the purpose of microscopic detection of pathology - non-cancerous skin diseases (for example, psoriasis, systemic lupus erythematosus, scleroderma, periarteritis nodosa, amyloidosis, skin tuberculosis, etc.), skin cancer, bacterial skin infections, fungal infections.
The results of the study are ready in 1-6 weeks. Scars can become a complication of this method, but in some cases a biopsy is simply necessary to obtain an accurate analysis and prescribe effective treatment.
Conditions for sample collection and storage
A clinical blood test is performed from venous blood stabilized with potassium salt EDTA, unless otherwise specified in the instructions for the analyzer. Blood collection is performed on an empty stomach. The blood sample should be mixed immediately after collection 9 times by gentle inversion, foam formation and sudden shaking should be avoided. Before testing, the blood sample can be stored at room temperature (23–24 °C) for 24 hours in a rack, in an upright position, away from light.
When using a capillary blood sample for clinical analysis, it is necessary to obtain free-flowing drops of capillary blood from the prewarmed puncture area. Collecting capillary blood without squeezing a finger ensures the safety of cells. Applying pressure to the puncture area and collecting a sample from a cooled limb will distort the hemogram results. Capillary blood samples must be stabilized with potassium EDTA, so K3EDTA-treated capillaries should be used for sample collection. Samples can be stored at room temperature (23–24 °C) for 24 hours on a rack, in an upright position, away from light.
Hemoscanning of blood: how it is done
The microscope is connected to a video camera, which displays the image on the monitor and also makes it possible to take photographs and videos of interesting objects. It is known that blood performs very important functions in the body. First of all, blood is a transport system that connects the work of all organs and systems. Blood interacts with every cell of the body, delivering them oxygen, bioactive, nutrients, and removes waste products, toxins and waste products that cells release during their functioning. Blood transports immune cells to areas of inflammation or the introduction of foreign agents (infections, allergens), and delivers platelets to areas of bleeding. The condition and composition of the blood is reflected in all pathological processes that occur in the body - inflammatory, infectious, metabolic, immune, allergic, etc. In case of digestive disorders, the function of the excretory organs (kidneys, intestines, skin and lungs), with dysbacteriosis and parasitosis, the blood becomes acidified, overloaded with toxic substances and free radicals.
Features of dark-field microscopy
A characteristic feature of hemodiagnostics is obtaining a visual picture without preprocessing. An indispensable condition for successful analysis is microscopy using the “dark field” method, which records the most insignificant changes in the refractive power of the objects under study. To obtain objective information about living cellular structures, blood is examined using a dark-field microscope immediately after sampling from a finger, in the presence of the patient. After just 10–15 minutes, irreversible changes occur in the sample taken and laboratory indicators become uninformative. During phase-contrast microscopy, the appearance, size and functional state of blood cells are assessed, plasma inclusions and micro-objects are identified. The visualization process is automated by special software “Dianel®-Micro”, which connects the microscope and the computer into a single optical digital control system.
Plasma analysis
The liquid part of blood is plasma
, gives us a fairly large amount of information about the state of the internal environment of the body. The presence of various inclusions in it: cholesterol crystals, uric and orthophosphoric acid salts, bacteria, larvae, fungi and their spores, the rapid appearance of fibrin threads is an indication of a predisposition to the development of a particular disease. Cholesterol crystals form when lipid metabolism is disrupted. Failure of the digestive process, liver and pancreas function leads to hyperlipidemia, which over time leads to a pathological condition - hypercholesterolemia. Cholesterol crystallizes, adsorbs waste products and bacterial waste products on its surface, becomes fixed in the vessels and becomes the basis of atherosclerotic lesions. This can cause the development of cardiovascular pathology.
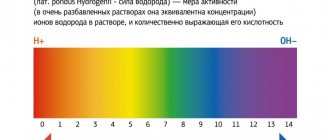
Leukocyte activity, eosinophil and basophil content
The state of the human immune system can be judged by the number, size, and activity of leukocytes
, quality composition. The presence of inactive, small cells, prone to grouping into groups of two or three, a decrease in the total number of leukocytes indicates a decrease in immunity, the presence of an inflammatory process (acute or chronic) in the body. An increase in blood pH inhibits the phagocytic activity of leukocytes and reduces the immunological response.
With an increase in the number of eosinophils and basophils
one can judge the predisposition to allergic reactions and the presence of parasitic infestation in the body.
What do orthophosphoric acid salts indicate?
Phosphoric acid salts
in the blood indicate a pronounced disturbance of phosphorus-calcium metabolism, calcium deficiency in the body, which again is a prerequisite for the development of various diseases. Phosphoric acid is formed during the disposal of proteins, heavy physical activity, consumption of products with thickeners, flavors, etc. Phosphoric acid is a “marker” of calcium loss. It saturates itself with calcium ions, and when the body removes it, it throws out the calcium accumulated in it along with it.
Presence of uric acid crystals in the blood
Presence of uric acid crystals
in the blood allows you to assess the level of protein metabolism in the body, the functioning of the kidneys and liver. Uric acid is a byproduct of protein digestion. As uric acid passes through the liver, it is converted into urea, after which the kidneys remove it from the body. Violation of protein metabolism leads to excessive formation of uric acid, its salts (urates), the formation of stones in the urinary tract, deposits in the joint capsules and articular surfaces.
What can the platelet count tell you?
Platelets
are cells of the blood coagulation system. Changes in the number, shape, and aggregation of platelets are signs of a violation of homeostasis: with blood loss, deregulation of the coagulation system, dehydration, pH shift to an acidic environment, acute infections, anemia, metabolic disorders, intravascular coagulation syndrome. An increase in the number of platelets and their aggregation is caused by provoking and contributing factors: hypokinesia, obesity, excessive physical activity, cooling, intravenous manipulation, taking hormonal contraceptives.