A separate disease called “ lack of air”
" does not exist. A feeling of shortness of breath is a symptom, a sign of a painful condition.
As stated above, there are two groups of reasons for this symptom:
1. Internal diseases: pathology of the heart, lungs, blood diseases, obesity, oncology, infections, injuries, etc.
2. Nervous and mental disorders:
- consequences of stress,
- prolonged or intense overload,
- neuroses,
- neurasthenia,
- panic attacks and other anxiety disorders,
- depression,
- consequences of organic damage to the nervous system,
- psychosomatic and somatoform diseases.
Statistics say that the vast majority of cases of feeling short of air when inhaling is a consequence of disturbances in the functioning of the nervous system.
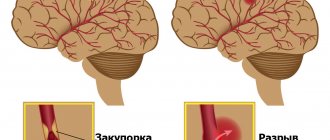
The mechanism for triggering this symptom is associated with the development of anxiety, overexcitation of the midline structures of the brain, excessive activation of autonomic centers, and the predominance of excitation processes over inhibition processes in neurons.
The feeling of shortness of breath may be accompanied by other symptoms:
- feeling of heartbeat,
- dry mouth or excessive sweating,
- feeling of heaviness in the chest or stomach,
- discomfort in the head and neck,
- internal trembling
- insomnia,
- loss of appetite,
- gastrointestinal disorders (diarrhea, constipation),
- fear of death.
Previously, doctors called such conditions VSD (vegetative-vascular dystonia), but in our time this term has ceased to be used.
Kinds
There are acute and protracted forms of vascular psychoses that arise against the background of existing non-psychotic mental disorders of vascular origin - pseudoneurasthenic manifestations and phenomena of intellectual decline of varying degrees (vascular dementia). However, first it is necessary to mention the symptoms that can serve as harbingers of vascular psychosis: increasing headaches, increasing tinnitus, numbness in certain areas of the face, impaired coordination of movements, dizziness, difficulty falling asleep, unstable mood with tearfulness and irritability (weakness). Speech becomes slurred and incomprehensible. Anxious fears of hypochondriacal content (fear of death or belief in the presence of a fatal disease) may appear. Patients may become more sloppy, gluttonous, and sometimes sexually disinhibited.
Acute form
The acute form is manifested primarily by phenomena of confusion with disorientation in time, surroundings, lack of recognition of others, often psychomotor agitation, influxes of visual and auditory hallucinations (essentially vascular delirium). Most often it develops in the evening or night hours, during the day the consciousness is clear. It usually lasts several hours, after the acute period amnesia develops - patients do not remember what they did during the exacerbation. This condition is prone to recurrence - repeated many times if the patient does not receive the necessary therapy. Very often, the plot of the experience is as follows: the patient believes that he is on a visit (to a hospital, a hotel), and at night he begins to get ready to go home; if the patient is inattentive on the part of his loved ones, he can actually leave home and get lost. Plots of hallucinations often involve meetings with deceased relatives. Additional factors provoking psychosis may be taking certain medications (cardiovascular, sleeping pills, Corvalol or Valocordin, a number of nootropics), fever, sharp fluctuations in blood pressure in any direction, diabetes mellitus. Some authors consider vascular delirium as one of the harbingers of an imminent stroke.
Protracted vascular psychoses
Protracted psychoses can develop as a transition from an acute state, or independently. The transition to protracted psychosis from an acute state can occur through a series of convulsive attacks, through the development of Korsakov psychosis with severe memory impairment (inability to record what is happening, replacement of memory loss with false memories), confusion, through the development of a pseudoparalytic state with carelessness, foolishness, ridiculous actions and ideas of grandeur or through severe asthenia (neuropsychic exhaustion).
Prolonged vascular psychoses most often occur as various variants of hallucinatory-delusional syndrome, that is, the main content of painful experiences is hallucinations and associated delusional ideas (false statements that cannot be dissuaded). Less often, they occur in the form of depression at a psychotic level (with or without anxiety) - patients feel deep sinfulness, for which there is no forgiveness, or a feeling that they have actually died and their body has already begun to decompose (Cotard's delirium). With various forms of vascular lesions of the brain, patients experience various additional symptoms.
Anger management. (Psychosomatics: hypertension, diabetes)
From the author:
Psychosomatics.
Anger. Probably no other topic arouses as much interest and enthusiasm as the topic of anger management. “You need treatment” is a common prescription for a person who shows his anger openly. Let's agree - in this article we are not considering cases of suppressed anger (more common in women and children). It is usually men who openly brawl.
Let's describe this feeling.
At first, as a rule, but not always, there is a feeling of irritation, which turns into indignation, then into anger, and finally into rage. Anger mobilizes a person’s energy, instills in him a feeling of confidence and strength, and suppresses fear.
Anger creates readiness for action. Perhaps in no other state does a person feel as strong and brave as in a state of anger. In anger, a person feels that his blood is “boiling,” his face is burning, his muscles are tense. The feeling of his own strength prompts him to rush forward and attack the offender.
And the stronger his anger, the greater the need for physical action, the stronger and more energetic the person feels. Emotions are an evolutionarily earlier mechanism for regulating behavior than reason.
Therefore, they choose simpler ways to solve life situations. E.I. Golovakha, N.V. Panina Anger is an emotion from the category of affects, which means that it can develop in a short time into a feeling of rage, which in its essence is very destructive and difficult to control.
Therefore, control over this feeling must be at the moment of its occurrence. “If an emotion is resolved, it comes out into the wild.” N. Kozlov If anger is not reacted externally, it does not disappear.
Being “swallowed” it transforms into resentment, irritation, apathy, etc.
Psychosomatic illnesses such as hypertension or diabetes mellitus, two of the most common illnesses associated with suppressed anger, may also occur.
An angry person has breakdowns regularly; emotional stress does not find an outlet in constructive ways of expression. A person gets into various fights and altercations, which, of course, does not contribute to prosperity in any area of life (everyone tries to avoid violent people), and besides, this is fraught with consequences.
What is the cause of anger?
1. The main reason for our anger is the pain caused to us. This is a natural reaction of the body, which has been brought to automaticity by evolution.
2.Anger can be a consequence of other feelings. For example, after feelings of sadness, shame, fear. In this case, we can talk about a response to emotional pain.
3. Anger can arise from your thoughts. For example, your assessment of another person’s actions. This could be unfair treatment, deception, violation of agreements, or disrespect.
If a person experiences anger, this indicates that he is not satisfying some important needs. Anger is a destructive feeling that gives a person a lot of energy. Negative energy literally begins to overflow, narrowing consciousness and adequate perception of reality, at the sight of an object of anger or mention of it. The issue of anger management is a matter of having the right beliefs and tools that help regulate this feeling.
It is necessary to move in order, since the correct order is the key to success in curbing this feeling :)
For anger management to become the norm, you need to remember a few basic rules:
12 main rules for managing anger
1. Decide to take control of your anger. Only by taking responsibility can you begin to make changes in your life. Also indicate why you need to manage this feeling, what opportunities and positive moments will appear thanks to this in your life.
2. Sustainable self-esteem. Take attacks in your direction as useful information. Don't take everything to heart. Find a solid foundation for your self-esteem.
3. Sports activities. Sports and any physical activity serve as an excellent preventive measure against anger. Moreover, you will learn to tolerate pain and tension, and this will give you extra points in mastering this feeling.
4. Recognize the warning signs. Try to observe yourself when you are irritated: you may notice that your lips, jaw or fists are clenched, your shoulders are tense, your eyebrows are furrowed, etc. By learning to recognize the early warning signs of an impending “storm”, you will gain time and will have time to take some action.
5. Learning to think in new ways. Our feelings are a reflection of our thoughts. For example, if you are used to thinking in a conflict situation something like “That’s it, I can’t do it anymore! I just can't stand it! How long can this continue!?”, then your emotional sphere reacts to such thoughts with an explosion of negative energy.
6. Tolerance and acceptance. One of the most destructive beliefs in our lives (mostly unconscious) is that everything should be the way we want it immediately. Try to tell yourself more often that other people are not there to meet your expectations about them. And also that events can develop according to their own scenario, regardless of what you consider “right” and “wrong”.
7. Soften the blow. Say to yourself in difficult moments, for example, when someone criticizes you or your neighbor’s house is undergoing renovations: “This is getting on my nerves, but it’s not fatal.” You will feel your own strength and will accept unpleasant events more calmly.
8. Reduce demands on others. Don't demand perfection from people. Highlight the main thing that is a priority for you, your life and your happiness. Constant “catching fleas” poisons the life of both you and those around you. Instead, think about what is truly important to you.
9. Justification. “He’s doing this on purpose to get at me” - don’t attribute bad motives to people. Even if a person really is planning something bad, then “he does it because he is unhappy, unloved and misunderstood.”
10. Anger management is largely the art of compassion. Switch mental places, look at the situation through his eyes. What do you see? Feel what he feels. What do you feel? Develop your ability to remember the good things about a person in a conflict situation. At least it will be objective.
11. Humor. A good joke can quickly defuse a situation. Think about how you could joke in typical situations that warm you up, and practice using your homework. Coming up with jokes when you're annoyed is much more difficult.
12. The result will come gradually. Anger management skills should be distinguished from knowledge about anger management skills. Acquiring them takes time and practice. You may know how to ride a bike, but not know how to do it until you start trying, and most importantly, keep trying, despite the inevitable failures. Don't be too hard on yourself: none of us are perfect.
There will definitely be breakdowns, but less and less often if you continue to educate yourself. Don't rush and don't beat yourself up for failures. Don't give up, and then everything will work out.
Many people have dramatically changed their lives by learning just three or four of these anger management techniques.
And so can you.
In addition to the general principles that will help you master the feeling of anger, it is important to have working instructions at hand, which, when practiced (at least 5-10 times), can become your skill and save you from a large number of problems.
So:
1. Admit to yourself that you are angry. Say out loud: “I’m very angry/angry! Acknowledgment is necessary to ensure continued, intelligent management of your emotions.
2. Use the STOP technique. When you feel the level of anger increasing, mentally tell yourself “STOP. After that, wait 5-10 seconds. At the moment when your emotions are ready to explode and burst into a storm against the offender, you get precious time to make the right decision in the current situation.
3. Inhale deeply several times. This will help restore breathing and heart rhythm. And also “ground yourself” and feel contact with the body again. “Blow off some steam”, in simple terms.
4. Put yourself in the shoes of the offender. Let's consider this situation. Let's say you were rude on public transport. The first reaction is to be rude in response. However, try to put yourself in the shoes of your offender. Maybe he has problems in his family, at work, or he is lonely and deeply unhappy. And he is rude not for the sake of pleasure, but unconsciously, due to a defensive reaction to more prosperous people than himself. Understanding that someone experiences pain when they are angry helps to develop compassion for the face rather than reacting with anger. This way you can take control of your negative emotions.
5. Choose several possible response options. Pausing gives you the opportunity to ask yourself the crucial question: What result do I want to get from this reaction?
6. Offer a solution. Focus on possible solutions to the problem and offer the person several options. Two or three options are better than one, as it gives your opponent a sense of freedom of choice. Use the wording – “What if. "Remember that anger is a bad helper in solving problems. Therefore, the best thing is to remain calm and balanced. When nerves are at their worst, it is better to try to keep your mouth shut. (Harris)
In the next article we will talk about sadness.
Sadness (an emotion that arises as a reaction to the failure of hopes, the inability to achieve a desired goal) is activated by similar shifts in neural activity, and the role of sadness is that it reduces the intensity of anger and the associated emotions of disgust and contempt.
I wish everyone good luck and success in working on themselves.
Sincerely, psychologist TANAILOVA VICTORIA VYACHESLAVOVNA
Write to email tel. +380986325205 tanaylova3
Hypertension Angina and queues in stores) - psychosomatics
Symptoms
With hypertension, there is always (even without psychosis) increased irritability at the slightest provocation, loss of self-control, self-criticism, and sense of humor. Previously ineffective stimuli (the noise of cars outside the window, the smell of cooking food, things that are not properly placed) cause intense discomfort. Mental fatigue and exhaustion increase; patients are unable to carry on a long conversation as before, watch an entire TV show, or read a newspaper or magazine to the end. They often become fussy, anxious, and often imagine possible misfortunes in their imagination for the slightest reason (a grandson is late from school, a daughter or son-in-law is unavailable by phone, a car accident was shown on TV, and so on). Attacks of sharp headaches with a feeling of excruciating pressure in the back of the head and frontal region, noise and ringing in the ears, and dizziness intensify. Fainting, blurred vision, numbness in the fingers, weakness in one half of the body, and sudden onset of deafness or blindness may occur. Psychotic states are more clearly defined in hypertension than in a pure atherosclerotic process. It is easier to identify the leading psychopathological syndrome and select adequate therapy.
Prolonged psychoses with hypertension tend to recur. In the later stages of hypertension, pseudoparalytic syndrome and Korsakov's psychosis, as well as anxious, melancholy and delusional states (delusions of harm, persecution, poisoning) can develop. And in a psychotic state, hypertensive patients continue to have particularly pronounced irritability and anger.
With a predominance of atherosclerotic brain lesions, various variants of prolonged psychoses have also been described. In many cases, they are extremely reminiscent of the picture of late schizophrenia due to special motor disturbances (catatonic syndrome), the specificity of hallucinatory-delusional experiences, pronounced apathy and indifference to the environment outside of exacerbation. For these psychotic states, the presence of polyvocal (several “voices at once”) true auditory hallucinosis, wave-like course, intensification of hallucinatory experiences in the evening and night hours, and predominantly threatening content of hallucinations are very typical. Such psychoses without treatment can last for years without the addition of automatisms, ideas of influence - this is how they differ from the schizophrenic process.
States of paranoia of vascular origin may also arise, for which a combination of delusional ideas of jealousy and damage is very typical. At the same time, the mood of patients is rather depressed than irritable or aggressive. In general, specialists experience significant difficulties in distinguishing prolonged depression in atherosclerosis from endogenous affective psychoses (manic-depressive psychosis, bipolar affective disorder), which first arise in old age in the presence of vascular disease. To establish the exact nature of depressive states, it is necessary to involve all data from the anamnesis, study the genetic background and personal characteristics of patients.
Get advice anonymously and free of charge
Our specialist will call you within 5 minutes, leave a request
Psychosomatics: cardiovascular diseases (hypertension)
From the author:
Notes on diseases related to psychosomatics
Diseases of the heart and blood vessels in economically developed countries are the most common cause of death. In recent years, cardiologists have increasingly attached importance to psychosocial risk factors and their relationship with somatic factors (Burns and Katkin, 1993; Burns et al. 1993; Cohen et al. 1994; Contrada, 1994; Dembroski, MacDougall, 1983; Miller et al. 1996). Lifestyle, personality attitudes and a person’s position in his professional and family environment are important for blood circulation and its physiological regulation. Somatic risk factors such as poor diet, obesity, smoking and alcohol abuse, which reflect personality characteristics, have long been known (Bräutigam et al. 1999).
The psychosomatic component is primarily characteristic of the following diseases of the cardiovascular system:
essential arterial hypertension; cardiac ischemia; heart rhythm disturbances; cardiac neurosis of fear.
The heart and blood vessels are involved in all forms of life, although normally a person is not aware of this. During physical and mental stress, the work of the heart begins to be perceived in the form of increased heartbeat or tachycardia. Unlike motor skills or breathing, the activity of the heart and blood vessels is excluded from direct human perception. And only in certain borderline states and disorders is the heart perceived consciously. Even in cases of severe disorders, for example with congenital heart disease, cardiac phenomena are subjectively perceived only in the later stages of decompensation. However, even in these cases, a kind of uncertainty arises: “although the heart is mine, it is somehow indefinite and cannot be controlled, like, for example, a limb.” This feeling of uncertainty already contains the germ of fear. This is the basis for the assumption about the possibility of phobic personality development.
The mental sphere also determines the functions of the heart and blood vessels, just like the somatic one. Activity and rest, sleep or wakefulness, mental alertness and excitement, externally expressed or suppressed feelings are associated with various states of the circulatory system. The connection between the activity of the heart and emotions is reflected in many idioms and sayings.
Despite the fact that changes in the functioning of the heart are equally manifested in both positive and negative feelings, pathological disorders in the cardiovascular system are associated with fear, anger, rage, melancholy and other negative emotions, which lead to the fact that, for example, fear of loneliness, in case of danger of attack, there is a feeling as if the heart begins to pound in the throat and in the head area. The resulting release of adrenaline causes vasoconstriction, increased heart rate and increased myocardial contraction, which, in turn, leads to a state of anxiety and fear.
The heart is usually associated with love.
The question arises: why does a break in a relationship or the loss of a loved one often lead to heart disease?
If a mother does not give her child enough warmth, he will show feelings towards his doll that he would like to feel in his mother. The doll becomes a substitute for a loved one. Some cardiologists suggest that sometimes the heart turns into a symbol of a loved one and all those feelings that for some reason cannot be expressed openly are transferred to it. A person is afraid to show others his dissatisfaction. A woman does not dare to object to her loved one and in order to reduce melancholy and avoid depression, she tyrannizes her own heart, taking out her irritation on it.
Repressed hostility plays a major role in the pathogenesis of cardiovascular diseases
(Barefoot et al. 1996; Barefoot et al. 1994; Benotsch et al. 1997; Siegman and Smith 1994; Siegman et al. 1992) and Type A behavior (Booth-Kewley and Friedman 1987).
Hypertension
Personality picture
Since in most cases it is not possible to clearly date the onset of the disease, it is difficult to talk about the situation causing it
.
However, certain internal conflicts have been described as causal situations
(Gentry, et al. 1982; Irvine, et al. 1991; Saab and Schneiderman, 1993).
Arterial hypertension often begins when a person is in a situation of chronic tense anticipation (Grace, Graham, 1952).
Typical statements of hypertensive patients: “I must be ready for anything”, “I am the type that takes on all the difficulties”, “no one can stop me, I am ready for anything.” Provoking situations are often prolonged states of fear, lack of time and increasing tension. In addition, situations are described in which there is a possibility of defusing hostility and aggressiveness, but this does not happen due to inhibition or scrupulosity. Numerous experiments with both animals and people have shown that blood pressure increases with fear, anger and bitterness and that chronic emotional overstrain can lead to persistent hypertension
(Coeher, 1971, Groen et al., 1971, Angermeier, Peters, 1973; Cannon, 1953; Reindell et al. 1971).
It is generally accepted that hypertensive patients have chronically suppressed aggression associated with fear.
For patients with hypertension, a typical neurotic personality structure is described with a predominance of obsessive states, as a result of which internal and external conflicts often arise, which makes emotional release difficult
(Groen et al.,1971).
The fact that essential hypertension often occurs in members of the same family can be interpreted in the sense of "psychological inheritance"
(Hermann et al.,1989). Experimental studies show that patients with hypertension are prone to increased blood pressure even in situations that do not cause any changes in blood pressure in normotensive patients (Hodapp, Weyer, 1982).
According to Alexander (2002), the central point of the psychodynamics of a patient with essential hypertension is the constant struggle with the growing hostile-aggressive feeling. At the same time, there are difficulties in self-affirmation. Patients are afraid of losing the favor of other people and therefore control the manifestations of their hostility. As children, they are usually prone to fits of rage and aggression. Previously an aggressive child, an adult becomes emphatically compliant and cannot stand up for himself. Understanding the possibility of losing the affection of family and friends because of one’s aggressiveness forces the child to control his hostility and hide it. Patients with arterial hypertension constantly show irritability if they encounter insurmountable resistance. Their life forces them into the role of a “draft horse.” They get stuck in one job for many years and rarely change companies, even if they are underpaid. If they achieve a position of authority, it is difficult for them to become an authority for others. They do the work for others instead of establishing discipline. From this hyper-conscientious and extreme behavior with an excessive sense of responsibility, intensified feelings of anger, hostility and aggressiveness are born, which over time require more and more effort to contain them. This develops a vicious circle that leads to a chronic state of tension. The characteristic situation that provokes the disease is life conflicts that mobilize hostility and the desire for self-affirmation and at the same time create the impossibility of their free expression.
Initially, these traits were discovered in the observed behavior of patients. Further studies showed that, in comparison with normotonics, their perception of conflict and stress is altered. For example, flight controllers are at risk of increased pressure not only when they identify with their profession and are adaptive and courteous to coworkers, but also when they fail to perceive and deny job stress (Rose et al. 1978).
Direct interaction in the family also plays a role in the formation of hypertension, as shown in studies of conflict behavior in families with a hypertensive father, in which the family was studied as a clinical unity, based on a systemic view of symptoms
(Baer et al. 1959, 1933; Baer 1983).
The personality structure of a family member—for example, the conflict-aggressive impulse of a hypertensive patient—affects the interaction behavior of the family as a whole (“family accumulation” of essential hypertension). In every family, rules are formed between parents and children by which conflicts are regulated; in families with a hypertensive father, children have less effective ability to tolerate and resolve conflicts, as evidenced by the predominance of negative nonverbal communication in these families (for example, not giving an answer, turning their head away, avoiding eye contact). A variety of studies indicate that a limited perception of conflict and stress and conflict avoidance correlates with the appearance of high blood pressure, i.e., these are types of behavior that children acquire in the process of socialization in the family from a hypertensive father. This view could, along with the genetic component, reveal a complementary aspect of the possible replication of essential hypertension (Theorell, 1990; Luban-Plozza et al. 2000).
Family interaction is characterized by a kind of prohibition on speech or communication, which also affects the non-verbal sphere, as a result of which understanding, observing, controlling, restraining activities predominate, while giving, reporting, participating expressions rarely appear (Kroger, Petzold, 1985).
A single personality structure for all patients with arterial hypertension has not been established. However, given the wide distribution and wide variety of forms of the disease, this should not be expected.
Yet, among psychosomatically examined pre-selected patients, certain personality traits recur consistently. Hypertensive people are described as hardworking, committed, sociable people, with a great sense of responsibility. In this regard, they have internal and external conflicts from which they cannot emotionally distance themselves. In their specific attitude of modesty, they give up their needs for the benefit of others, wanting to receive their approval and not provoke aggression or hostility. It is these signs, described independently of each other by different researchers as willingness to help, shyness, chronically suppressed aggressiveness, that make up the manifest personality traits, which are of great importance for the formation of characteristic reactions of suppressing needs perceived as dangerous. The manifest features of perception of the environment and behavior in many hypertensive patients are a form of defense against their own aggressive impulses (Cottington et al. 1986; Diamond, 1982).
Most patients with essential hypertension usually do not have proper awareness of their illness. From a psychoanalytic position, outwardly incorrect neurotic behavior is ideologically justified by the desire to be active and help people. But even with this unfavorable initial situation, in some cases it is possible to achieve changes if, thanks to the maturation of the personality, its one-sided direction is eliminated and the person as a whole begins to navigate life in a new way.
Manifest personality traits of a patient with arterial hypertension
. His hard work and orderly behavior, contact, accuracy and conscientiousness are impressive, making him a seemingly pleasant, compliant patient. However, it should be remembered that in most cases a hypertensive patient does not verbalize his aggressiveness, ambition and desire for competition, which often remain latent. This can be felt if you try to have a lasting influence on the patient's lifestyle. Its low compliance with the necessary long-term therapeutic program, during which the patient usually cannot realize his needs and cannot even express his judgments and attitudes that are contrary to the therapeutic program, often complicates the relationship between the psychotherapist and the patient. In work and family crisis situations, and especially in latent conflicts in relationships with a psychotherapist, patients are easily vulnerable, but cannot verbally express their aggressiveness. They simply leave treatment and do not appear on time. This seemingly unmotivated interruption of treatment leads to the development of a feeling of guilt and its projection. It is important for the psychotherapist to countertransference that he is aware of his patient's oppositional tendencies and encourages him to talk, helping him cope with feelings of guilt or tension during treatment. A benevolent attitude, in which the therapist himself does not feel disadvantaged and does not make unnecessary reproaches, determines the possibility of continuing therapy.
For the relationship between the psychotherapist and the patient, it is important to notice in time that the patient tends to suppress his own critical needs and identify them only indirectly, for example, in the form of an unmotivated interruption of treatment.
Psychotherapy
The relationship between the psychotherapist and the patient is often characterized by a conflict of aggressiveness/dependence on the part of the patient.
Conditions for the treatment of hypertension are characterized by:
- low motivation, since complaints are received mainly about minor subjective symptoms;
— good possibilities of drug therapy;
— personal factors characterized by a conflict of aggressiveness/dependence, which can lead to tension in the relationship between the therapist and the patient and be expressed in unreliable interaction.
For supportive treatment, early involvement of the social field, a non-directive attitude of the psychotherapist towards the patient that does not activate the conflict of aggressiveness/dependence, active communication of information by the psychotherapist, strengthening of one’s own responsibility and independence, as well as self-perception (for example, through self-measurement of pressure) are recommended.
Psychotherapeutic treatment seems appropriate and indicated only when the patient has the appropriate level of suffering. Relaxation and behavioral techniques are well established as a means of supporting drug therapy, as they can significantly reduce drug doses.
As part of a behavioral therapy program, the patient's own responsibility should be achieved through the use of biofeedback and stress-relief techniques. Patients must understand what situations, difficulties, and conflicts lead to increased blood pressure, and learn to control their successes and failures. It is necessary to clarify whether these successes correspond to the canons of the classical reflex theory and whether we are talking about the direct formation of conditioned connections, and not just about teaching patients general sedative techniques.
Methods of solution-focused therapy, symbol drama, art therapy, creative visualization, transactional analysis, and family psychotherapy can be successfully used.
Litvinova Angelina Sergeevna
Litvinova Angelina Sergeevna is not the author of the text of this note.
Treatment of vascular psychoses
Treatment of psychosis is best started with treatment of the underlying vascular disease that caused the psychosis. Prescription of antipsychotic drugs (neuroleptics) is mandatory. For greater safety and effectiveness of treatment, it is best to select an antipsychotic drug in the clinic, then continue taking the drug on an outpatient basis. It is also necessary to prescribe vitamins, restorative drugs, neuroprotectors and vascular agents. Preventive measures to prevent the occurrence and recurrence of vascular psychoses: timely diagnosed vascular disease; establishing a constant and orderly daily routine; preventing excessive emotional stress; giving up smoking, alcohol and other bad habits; proper, balanced nutrition; giving up a sedentary lifestyle; physical therapy classes; Constant monitoring of blood pressure, cholesterol and blood glucose levels.
Hypertonic disease
Treatment of hypertension (illustration)
Ekaterina V. (38 years old) has been forced to constantly take antihypertensive drugs due to high blood pressure over the past 3 years. She underwent a special examination, as a result of which she was diagnosed with hypertension. She herself understands that the disease developed on a nervous basis - due to excessive psychological stress at work. Ekaterina is the director of a successful private company. Work is actually not time-regulated, so production issues have to be resolved not only in the office, but also at home. Lives with his elderly father in a three-room apartment. Her sex life is limited to infrequent intercourse with an elderly married man whom she has known for more than 10 years. The love that once brought them together has long passed, but the sexual partnership continues to be stereotypically pleasant.
This story has a happy ending. As a result of the treatment, the patient managed, firstly, to master the role of an adult woman; secondly, find a lover among your colleagues and marry him; thirdly, to conceive and give birth to a child, and shift the role of director to her husband. The remarkable thing is that the increase in hypertension during pregnancy predicted by the gynecologist not only did not happen, but on the contrary, blood pressure returned to normal.