Nitroglycerin
In acute myocardial infarction or acute heart failure, it should be used only with careful clinical monitoring of the patient.
To prevent an increase in angina attacks, abrupt withdrawal should be avoided.
If the patient is known to be taking phosphodiesterase-5 inhibitors, drug therapy is contraindicated. Patients receiving therapy with the drug should be warned not to take phosphodiesterase-5 inhibitors (for example, sildenafil, tadalafil, vardenafil).
Against the background of intravenous administration of the drug, a significant decrease in blood pressure and the appearance of dizziness may occur during a sharp transition from the “lying” or “sitting” position to the “standing” position; hot weather, as well as increased angina (with a sharp decrease in blood pressure) and myocardial ischemia up to myocardial infarction and sudden death (paradoxical nitrate reactions). To prevent an undesirable decrease in blood pressure, the rate of drug administration should be individually and methodically selected correctly. A decrease in blood pressure can be observed not only during the period of selecting the rate of drug administration, but also later against the background of stabilized blood pressure. Therefore, blood pressure monitoring should be carried out at least 3-4 times per hour throughout the entire infusion time.
It is possible to develop tolerance and cross-tolerance to other drugs of the nitrate group with long-term use, especially in high doses. Patients previously treated with organic nitrates (eg, isosorbide dinitrate, isosorbide-5-mononitrate) may require a higher dose.
If blurred vision persists or is severe, treatment should be discontinued.
In patients with severe liver failure and severe renal failure, dose adjustment is required depending on the severity of the disease (especially when using high doses), it is recommended to start with the lowest possible dose. Careful monitoring of the patient is necessary.
Hypoxemia
Caution should be exercised when used in patients with arterial hypoxemia due to severe anemia (including glucose-6-phosphate dehydrogenase (G6PD)-induced deficiency) because the metabolism of nitroglycerin is reduced in such patients.
Caution is also required when used in patients with hypoxemia and impaired ventilation/perfusion due to pulmonary disease or heart failure; as well as in patients with angina pectoris, myocardial infarction or cerebral ischemia, with airway disorders (especially alveolar hypoxia).
Under these conditions, vasoconstriction occurs in the lungs in order to shift the perfusion of the area of alveolar hypoxia to the part of the lung with better ventilation (Euler-Lillestrand reflex). As a potent vasodilator, nitroglycerin may interfere with this protective vasoconstriction and consequently lead to increased perfusion of poorly ventilated areas, worsening venous-perfusion imbalances, and a further decrease in arterial partial pressure of oxygen.
Methemoglobinemia
The development of methemoglobinemia has been reported after use of the drug. Treatment of methemoglobinemia with methylene blue is contraindicated in patients with glucose 6-phosphate dehydrogenase or methemoglobin reductase deficiency.
Intravenous nitroglycerin in the treatment of acute coronary syndromes
The continuing increase in morbidity and mortality from cardiovascular diseases is one of the most important factors influencing the formation of an unfavorable demographic situation in Russia. According to experts, mortality from diseases of the circulatory system will increase.
In the structure of causes of overall mortality in Russia, diseases of the circulatory system account for 55.6%. According to the State Statistics Committee of Russia, 1,253,102 people died from pathologies of the circulatory system in 2001, while in 2002 - already 1,302,202. More than 1.2 million people die every year as a result of cardiovascular diseases.
The most vulnerable category of the population susceptible to cardiovascular disorders (CVD) is the age group from 20 to 29 years. It is in this group that a significant increase in mortality is observed (from the report of the Minister of Health of the Russian Federation “On the results of the work of health authorities and institutions in 2002 and measures to improve the quality of medical care to the population”).
Thus, one of the main tasks of healthcare and cardiology in particular is to reduce overall mortality throughout the Russian population, and especially mortality among young working people.
One of the ways to solve this problem is the timely and reasonable use of medicines, including nitro-containing drugs. The most effective therapeutic drug is the ampoule form of nitroglycerin.
A pronounced and quickly manifested anti-ischemic effect, an equally pronounced and rapid effect on hemodynamics, “controllability” and safety - all these characteristics of nitroglycerin (NTG) have long allowed it to take its place among the main drugs used to treat exacerbations of coronary heart disease (CHD; see Table 1). This report contains modern recommendations for the use of intravenous NTG in the treatment of patients with acute coronary syndromes (ACS).
| Table 1. Dosage forms of NTG recommended for the treatment of ACS. |
Mechanism of action: antianginal, hemodynamic and other effects of NTG
The mechanism of action of NTG and other nitrates is closely related to one of the main vasoactive substances in the body - nitric oxide. Essentially, all nitrates should be considered as exogenous sources. Nitric oxide, by activating the enzyme guanylate cyclase, helps to increase the content of cyclic guanidine monophosphate (cGMP) in cells, a universal intracellular messenger that causes relaxation of smooth muscle structures.
The antianginal effect of NTG is based on multiple physiological reactions, caused both by its direct effect on coronary blood flow and by changes in a number of hemodynamic characteristics. By causing dilation of normal and atherosclerotic arteries and increasing blood flow in collaterals, NTG improves coronary circulation and promotes blood redistribution in favor of the ischemic area. IGT causes predominantly venous as well as arterial dilatation. By dilating the peripheral veins, NTG reduces the level of preload, which, in turn, reduces the tension of the left ventricle and its oxygen demand. By dilating peripheral arteries, NTG reduces afterload.
In addition to the listed vascular effects of NTG (especially pronounced when administered intravenously), mention should be made of the beneficial effects on the parameters of the coagulation system, the aggregation of blood platelets, and the rheological properties of blood.
There are a number of imported drugs for intravenous nitroglycerin on the drug market in Russia (perlinganite, isoket, nitromac, nitroject, etc.), and a domestic drug has recently appeared - “Nitroglycerin solution 0.1% for injection No. 10”. Domestic intravenous nitroglycerin is not inferior to imported analogues and practically does not cause side effects, which is due to the absence of alcohol in its composition (the drug is an aqueous, not an alcoholic solution) and a low glucose content - 0.1%.
NTG in the treatment of ACS from the perspective of evidence-based medicine
Conducted by S. Yusuf et al. [10] a meta-analysis of 10 small randomized studies performed in the period preceding the widespread use of thrombolytic therapy in the treatment of acute myocardial infarction (MI), and including a total of about 2000 patients, showed a fairly pronounced (35%) reduction in mortality in patients who received early intravenous introduction of NTG. The most serious and large-scale controlled studies of nitrates in acute MI were performed in the early 90s. last century - GISSI-3 [2] and ISIS-4 [3]. They already included the use of thrombolytic agents. In fact, both studies, covering about 80 thousand patients, compared the effectiveness of two strategies - routine (“all in the absence of contraindications”) and selective (“according to indications”) use of nitrates in the treatment of acute MI.
In this regard, it is not entirely correct to interpret their results “traditionally,” i.e., as evidence that nitrates do not affect the survival of patients with MI. It is probably more acceptable to conclude that there is no advantage to routine use of nitrates over selective use, since a significant proportion of patients randomized to the “control group” naturally received nitrates when needed. There have been no significant studies of the effectiveness of nitrates in unstable angina and non-ST elevation MI (non-ST elevation ACS). Thus, the use of NTG and other nitrates in patients with ACS, as modern authors unanimously note, is based mainly on “pathophysiological premises and clinical experience” [4].
Indications for starting intravenous administration of NTG in patients with ACS
Intravenous infusion of NTG in ACS with ST segment elevation
Indications for starting intravenous infusion of NTG in patients with MI are presented in Table 2 and correspond to the main provisions of existing practical guidelines [5]. Conditions in which NTG infusion is effective during the first 24-48 hours include cases of anterior major MI; MI complicated by heart failure and recurrent ischemia; MI occurring against the background of high blood pressure (BP). Infusion of NTG can last more than 48 hours with persistent stagnation in the pulmonary circulation and early post-infarction angina. There are no restrictions for the routine use of NTG in all cases of MI (in the absence of contraindications), as well as (for more than 48 hours) in cases of extensive anterior MI complicated by heart failure.
Intravenous infusion of NTG for ACS without ST segment elevation
The need for intravenous administration of NTG in cases of ACS without ST elevation (see Table 3) is largely determined by the presence of clear indications. As a rule, its use is advisable in patients with high coronary risk - with recurrent angina attacks, despite adequate treatment, as well as in cases of congestive heart failure.
Contraindications to starting intravenous infusion of NTG
Conditions in which the use of intravenous NTG may be associated with potential risks (see Tables 2, 3) include arterial hypotension with a systolic blood pressure level below 90 mm Hg. Art., bradycardia (heart rate less than 50 per minute) or, on the contrary, severe tachycardia. Contraindications should also include right ventricular myocardial infarction, which occurs with significant hemodynamic disturbances. Nitrates are unsafe for patients who have used sildenafil (Viagra) within the next 24 hours. The last warning is due to the mechanism of action of sildenafil, which blocks phosphodiesterase and thereby promotes excessive accumulation of cGMP in cells. This can lead to the development of uncontrolled arterial hypotension with all the ensuing consequences.
Dosing of intravenous NTG, development of tolerance
If necessary, the administration of NTG can be started with an intravenous bolus of 12.5-25 mcg. The initial infusion rate is usually 10 mcg/min. At intervals of 3-5 minutes, monitoring the patient’s condition, the infusion rate is increased by 10 mcg/min until individual criteria for optimal dosing are achieved. These include: elimination of ischemic symptoms, reduction of systolic blood pressure by 10% (10-15 mm Hg) in patients with normal blood pressure and by 25-30% in patients with high blood pressure. The criterion for optimal dosing of NTG in congestive heart failure is, as a rule, the blood pressure level. There is no information on the maximum permissible doses of IGT, although in practice doses exceeding 200 mcg/min are usually not used. If the symptoms of ischemia are not eliminated by increasing the rate of NTG administration, then the criterion for stopping further increase in the dose is the blood pressure level.
The development of tolerance to IGT becomes clinically significant one day after the start of continuous infusion. In ACS, tolerance is usually not a major problem and can be overcome by escalating the dose of the drug administered. If longer-term use of nitrates is necessary, conditions should be created for their administration in intermittent courses, using alternative treatment options.
Side effects of intravenous NTG and discontinuation of its infusion
The most common side effects of intravenous NTG infusion are hypotension and headache. Methemoglobinemia, as a rule, has only theoretical significance: it has been shown that even long-term (two to four weeks) administration of NTG at 300-400 mcg/h does not lead to an increase in the content of methemoglobin in the blood [6]. The most serious side effect of IGT is considered to be arterial hypotension. A pronounced decrease in blood pressure upon administration of even minimal doses of NTG may be one of the clinical manifestations of right ventricular myocardial infarction.
If necessary, an attempt is made to gradually reduce the infusion rate (especially in patients receiving large doses of the drug) with subsequent cessation of the administration of NTG. Rapid abolition of IGT in some cases can provoke repeated ischemic attacks.
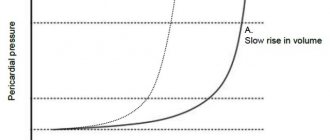
IGT and right ventricular myocardial infarction
Typical disorders that develop with significant lesions of the right ventricular myocardium are characterized by dilatation of its cavity, a decrease in right ventricular output, a decrease in left ventricular preload, left ventricular filling pressure, cardiac output, circulating blood volume and systemic blood pressure. Due to the above reasons, a further decrease in preload with the introduction of NTG and diuretics can lead to worsening hemodynamic disorders, arterial hypotension, and even the development of shock. The basis for the treatment of shock that complicates the course of right ventricular myocardial infarction is volume-replenishment therapy and the use of dobutamine. With combined dysfunction of the left and right ventricles, NTG infusion may be added to treatment with dobutamine; in this case, manipulations of administered drugs are optimally carried out under the control of central hemodynamic parameters using a “floating” Swan-Ganz catheter. The maximum indicators of the pumping function of the heart are usually observed when the “jamming” pressure increases to 20 mm Hg. Art.
NTG in the treatment of patients with cardiogenic shock
Dopamine and/or dobutamine, drugs that stimulate cardiac contractility and have a pressor effect, form the basis of pharmacotherapy for cardiogenic shock. Carefully monitored infusion of NTG may be required if there is a need to further reduce left ventricular filling pressure, increase cardiac output, or when pulmonary congestion is associated with the use of pressor agents.
Summarizing all of the above, we can conclude that in the absence of clear contraindications and compliance with all necessary precautions, intravenous NTG can be actively used in the treatment of various forms of ACS, including MI.
An important advantage of NTG for intravenous administration, which distinguishes it from other nitrates, is its greater safety, determined by the pharmacokinetics of this drug (rapid onset of action, short half-life), which makes it possible to very quickly stop the effect of NTG if adverse events develop. In addition, this makes it possible to regulate the degree of therapeutic effect of NTG. Due to its good “controllability,” intravenous NTG in the early stages of acute coronary disorders should be given preference over its other dosage forms (sublingual, tablets, aerosol).
Tolerance that develops with prolonged NTG infusion is usually easily overcome by increasing the dosage or rate of administration.
S. V. Shalaev, Doctor of Medical Sciences, Professor Medical Academy, Tyumen
Literature
- Yusuf S., Collins R., MacMahon S. et al. Effect of intravenous nitrates on mortality in acute myocardial infarction: an overview of the randomized trials. Lancet 1988;1:1088-92.
- GISSI-3: Gruppo Italiano per lo Studio della Sopravvivenza nell, Infarto miocardico. Effects of lisinopril and transdermal glyceryl trinitrate singly and together on 6-week mortality and ventricular function after acute myocardial infarction. Lancet 1994;343:1115-1122.
- ISIS-4 (Fourth International Study of Infarct Survival) Collaborative Group. ISIS-4: a randomized factorial trial assessing early captopril, oral mononitrate, and intravenous magnesium sulphate in 58,050 patients with suspected acute myocardial infarction. Lancet 1995;345:669-85.
- Bertrand ME, Simoons ML, Fox KAA, et al. Recommendations of the Task Force of the European Society of Cardiology. Management of acute coronary syndromes: acute coronary syndromes without persistent ST segment elevation. Eur. Heart J 2002;23:1809-40.
- Ryan TJ, Antman EM, Brooks NH, et al. 1999 Update: ACC/AHA guidelines for the management of patients with acute myocardial infarction: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). Circulation 1999;100:1016-30.
- Braunwald E, Antman EM, Beasley JM, et al. ACC/AHA guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients with Unstable Angina) . 2002. Available at https://www.acc.org/clinical/guidelines/unstable/unstable.pdf
The place of intravenous nitrates in modern cardiology
In 1879, W. Murrell reported the possibility of stopping an attack of angina by taking nitroglycerin. Since that time, the intensive use of nitrates in the clinic of internal diseases began. Until the advent of beta-blockers and calcium channel blockers, they were the only representatives of antianginal drugs in the cardiologist's arsenal.
Table 1. Sequence of actions for the development of tolerance to nitrates against the background of their continuous infusion (6)
Table 2. Contraindications to the administration of nitrates for AMI (30)
The emergence of intravenous forms of nitrates allowed them to take a leading position not only in planned, but also in emergency cardiology. Currently, nitroglycerin (for example, Perlinganite, Schwarz Pharma AG) and isosorbide dinitrate (for example, Isoket, Schwarz Pharma AG) are produced in forms for intravenous administration.
The mechanism of action of nitrates is associated with their venodilating properties. In this case, blood is deposited in the veins and the preload on the heart decreases, diastolic pressure decreases, the degree of mechanical stress on the walls of the ventricles decreases, and the myocardial oxygen demand decreases.
Unstable
angina
The use of nitrates in the treatment of unstable angina is associated with a pronounced antianginal effect. Mikolich et al. reported complete relief of pain in 89% of patients with unstable angina already when using a starting dose of nitroglycerin (5-10 mcg/min); with a further increase in it, pain symptoms were completely reduced in 98% of patients (1). However, clinically significant side effects (hypotension) developed in only 1% of patients (1). Similar results were obtained by other authors (2-5). In all cases, nitrate infusion effectively relieved pain; the infusion rate varied from 5 mcg/min to 200 mcg/min. Side effects not related to hypotension - headache, nausea, vomiting - occurred extremely rarely.
If the infusion lasts more than 24 hours, tolerance to nitrates usually develops. The algorithm of action for the development of tolerance to nitrates is given in Table 1.
There is evidence that infusion of isosorbide dinitrate for unstable angina allows some degree of avoidance of the adverse effects observed with nitroglycerin therapy (5, 7).
Thus, in case of unstable angina, the administration of intravenous nitrates promotes complete relief of pain as early as possible, which leads to a significant improvement in the patient’s clinical condition (8, 9).
Intravenous nitrates also improve long-term outcomes. A randomized comparative study of intravenous diltiazem and nitroglycerin for unstable angina showed that, within a year of continuous 48-hour infusion, the incidence of cardiovascular events after the use of nitroglycerin in high-risk patients was significantly reduced in both groups (10).
Interesting data were obtained by Doucet et al when comparing the effectiveness of intravenous nitroglycerin and heparin in patients with unstable angina due to restenosis after coronary angioplasty. The authors randomized 200 patients hospitalized within 6 months of angioplasty (without stent placement) to double-blind therapy (intravenous infusion) with nitroglycerin, heparin, their combination, and placebo for a total duration of 63,630 hours. Recurrent angina attacks occurred in 75% of patients in the placebo and heparin groups, compared with 42.6% of patients in the nitroglycerin group and 41.7% in the nitroglycerin plus heparin combination group ( P
PP = 0.0001) for nitroglycerin compared with no nitroglycerin and 0.98 (95% CI, 0.55–1.73,
P
=NS) for heparin compared with no nitroglycerin.
It is considered necessary to prescribe intravenous forms of nitrates if the pain syndrome is not completely relieved after using sublingual forms three times. However, in specialized departments it is recommended to immediately start intravenous infusion (if there are no contraindications to the use of drugs of this group) (12, 13).
Acute
myocardial
infarction (AMI)
In 1988, Yusuf et al. Conducted a meta-analysis of randomized trials on the use of intravenous nitrates in acute myocardial infarction (based on more than 2000 patients) (14). It was found that with this form of therapy, mortality in the first week after AMI is reduced by 35%. The divergence of survival curves continued up to 7 months, and after this period the differences were not significant. At the same time, the beneficial effect on short- and medium-term prognosis was higher in patients who suffered anterior AMI. Therefore, intravenous administration of nitrates in the acute phase of AMI in patients who have not received thrombolytic therapy has a beneficial effect not only on in-hospital mortality, but also on medium-term parameters.
A meta-analysis of randomized trials on the use of nitrates for AMI in the “era” of thrombolytic therapy was carried out in 1996 by Hennekens et al. It included 22 studies: 11 small studies using intravenous formulations, 9 small studies using oral formulations, and the results of the multicenter, randomized, double-blind studies ISIS-4 and GISSI-3.
The ISIS-4 study included 58,050 people admitted to hospital within the first 24 hours after the onset of clinical symptoms. Patients were prescribed controlled-release oral isosorbide mononitrate (initial dose 30 mg, titrated to 60 mg once daily) or placebo for four weeks. A decrease in mortality on day 35 was found to be 3% (not statistically significant) (15). Therapy with oral nitrates reduced the intensity of pain, did not affect the incidence of cardiogenic shock, and was associated with headache and hypotension, which required discontinuation of nitrate therapy.
The GISSI-3 study (16) included 19,394 people admitted to hospital within the first 24 hours of symptom onset. Patients received either an intravenous infusion of nitroglycerin (initial dose 5 mcg/min, titrated until systolic blood pressure decreased by 10%) for 24 hours, and then switched to the use of transdermal forms (10 mg/day) or they were prescribed the usual standard therapy.
In the nitrate group, a decrease in overall mortality by 6% (statistically unreliable), a decrease in the incidence of post-infarction angina (P
Intravenous forms of nitrates are the only antianginal drugs in the specialist’s arsenal in case of AMI development due to cocaine consumption. As is known, the use of beta-blockers in this case is strictly prohibited due to excessive stimulation of alpha-adrenergic receptors and further aggravation of the clinical situation (22). In this category of patients, intravenous infusion of nitroglycerin (23) or isosorbide dinitrate (24) completely relieves anginal pain and prevents the development of complications of AMI. It should also be noted that most of the studies were carried out in patients with elevated central venous pressure and stable hemodynamic parameters.
Intravenous administration of nitrates has been successfully used for complicated myocardial infarction. Bulus administration of nitroglycerin during pulmonary edema against the background of AMI allows not only to relieve the symptoms of acute heart failure, but also has a beneficial effect on the further course of the disease (25). In some cases, the use of intravenous forms of nitrates in cardiogenic shock is justified (26, 27), although no randomized studies have been conducted on this issue. Nitroglycerin has an advantage over other vasodilators because it does not cause coronary steal syndrome (19). Nitroglycerin is of particular importance in cardiogenic shock against the background of acute mitral regurgitation27. Particular attention should be paid to monitoring hemodynamic parameters.
The choice of nitrates for infusion therapy for AMI is as follows. Nitroglycerin has a quick and short-lasting effect and is easy to administer. Therefore, it has an advantage in patients with unstable hemodynamics. The rapidly occurring antianginal and hemodynamic effects make it possible to recommend it also in the presence of left ventricular failure. The possibilities of its use are limited by rapidly developing tolerance (Table 1). In all other cases, preference is given to isosorbide dinitrate (14, 28, 29).
Intravenous infusion of nitrates is indicated for all patients with AMI in the presence of myocardial ischemia, arterial hypertension, and heart failure. Nitroglycerin infusion is carried out at an initial rate of 5-10 mcg/min. If well tolerated and clinically necessary, the dose is titrated by 5-15 mcg/min until the existing clinical symptoms are relieved or the mean arterial pressure decreases by 10%. In this case, systolic blood pressure can decrease by no more than 30 mm Hg. Art. from the original values.
The initial rate of isosorbide dinitrate is 25 μg/min. It is titrated according to the parameters given above in increments of 25 mcg/min. It should be remembered that at a dose of both nitroglycerin and isosorbide dinitrate above 200 mcg/min, their further use is inappropriate, since in this case we can talk about existing resistance to nitrates.
With recurrent myocardial ischemia, it is possible to repeat the infusion of nitrates according to the same schemes. However, it is almost always necessary to use a higher dosage due to the development of tolerance.
Table 2 shows contraindications to the prescription of nitrates for AMI.
Acute
heart failure
Currently, several randomized studies have proven the effectiveness of intravenous administration of nitrates together with furosemide. However, titration of nitrates to the maximum tolerated dose and low doses of furosemide have been shown to be a preferable treatment for acute heart failure compared with high doses of furosemide and low doses of nitrates (grade I recommendation, level of evidence B) (31).
One of these randomized studies demonstrated that intravenous infusion of isosorbide dinitrate was more effective in reversing severe pulmonary edema compared with furosemide (32). Relief of pulmonary edema by intravenous administration of nitroglycerin is effective (33, 34).
When treating acute heart failure with nitrates, one should remember their U-shaped action. They are ineffective when used at submaximal doses, and high doses are also unable to relieve clinical symptoms (31). Nitroglycerin infusion should be carried out at a minimum rate of 20 mcg/min, increasing the dose to 200 mcg/min if necessary. The starting dose of isosorbide dinitrate is 1 mg/hour, titrated to 10 mg/hour if necessary.
Hypertensive
crisis
Intravenous forms of nitrates are indispensable for complicated hypertensive crises in the presence of left ventricular dysfunction or myocardial ischemia. Nitroglycerin has been shown to be as effective as sodium nitroprusside in these conditions (35). Due to their predominant venodilating effect, nitrates cannot be considered as a first-line treatment for relieving a hypertensive crisis, however, in case of damage to target organs, in particular the heart, their importance cannot be overestimated (36).
Other
points of application of intravenous forms of nitrates
In patients after coronary artery bypass surgery, intravenous administration of nitrates helps reduce coronary vasospasm (37). Intravenous nitroglycerin has been used successfully to maintain normal cardiac function in patients awaiting cardiac transplantation (38), to prevent reperfusion injury after heart and lung transplantation (39), and to prevent stress-induced arrhythmias in patients with coronary artery disease (40). .
Current
issues in the use of intravenous forms of nitrates
Previously, one could find indications in the literature that the combined use of nitrates and heparin reduces the effectiveness of the latter. Specially conducted studies have shown that for doses of nitrates used in emergency cardiology, their interaction with heparin is not clinically significant (41, 42).
A significant number of intravenous forms of nitrates are alcohol solutions, while the volume and weight fraction of ethyl alcohol in some of them can exceed 80-90%. To improve the safety profile and tolerability, aqueous solutions of nitroglycerin (Perlinganite, Schwarz Pharma AG) and isosorbide dinitrate (Isoket, Schwarz Pharma AG) should be used. To increase efficiency, it is necessary to use intravenous systems made only from polyethylene and polypropylene.
Intravenous forms of nitrates are highly effective and safe drugs, widely used in emergency cardiology. Low cost and ease of use make drugs in this group even more attractive and profitable.
Nitroglycerin 0.1% 10ml n10 solution for injection
Release form
Tablets, capsules and sublingual drops.
Compound
Capsules and tablets of 0.5 mg nitroglycerin.
Drops 10 mg/ml.
Package
20, 40 pcs.
pharmachologic effect
NITROGLYCERIN is a peripheral vasodilator with a predominant effect on venous vessels. Antianginal agent. The mechanism of action is associated with the release of the active substance nitric oxide in the smooth muscles of blood vessels. Nitric oxide causes activation of guanylate cyclase and increases cGMP levels, which ultimately leads to smooth muscle relaxation. Under the influence of nitroglycerin, arterioles and precapillary sphincters relax to a lesser extent than large arteries and veins. This is partly due to reflex reactions, as well as the less intense formation of nitric oxide from active substance molecules in the walls of arterioles.
The effect of nitroglycerin is mainly associated with a decrease in myocardial oxygen demand due to a decrease in preload (dilation of peripheral veins and a decrease in blood flow to the right atrium) and afterload (decreased peripheral vascular resistance). Promotes the redistribution of coronary blood flow into ischemic subendocardial areas of the myocardium. Increases exercise tolerance in patients with coronary artery disease and angina pectoris. In heart failure, it helps to unload the myocardium mainly by reducing preload. Reduces pressure in the pulmonary circulation.
Indications
IHD: angina pectoris (treatment, prevention), vasospastic angina (Prinzmetal), unstable angina, spasm of the coronary arteries during coronary angiography, acute coronary syndrome, acute myocardial infarction, acute left ventricular failure (cardiac asthma, interstitial and alveolar pulmonary edema), chronic heart failure, controlled arterial hypotension during surgical procedures, prevention of hypertensive reactions during endotracheal intubation, skin incisions, sternotomy, occlusion of the central retinal artery, esophageal dyskinesia, functional cholecystopathy, acute pancreatitis, biliary colic, spastic intestinal dyskinesia.
Contraindications
Hypersensitivity, severe hypotension, collapse, myocardial infarction with low end-diastolic pressure in the left ventricle and/or severe hypotension (systolic blood pressure below 90 mmHg) or collapse, right ventricular infarction, bradycardia less than 50 beats/min, primary pulmonary hypertension, cerebral hemorrhage, head injury, increased intracranial pressure, cerebral ischemia, cardiac tamponade, toxic pulmonary edema, severe aortic stenosis, conditions accompanied by a decrease in end-diastolic pressure in the left ventricle (isolated mitral stenosis, constrictive pericarditis), angle-closure glaucoma, pregnancy, breastfeeding.
Directions for use and doses
Orally, sublingually, buccally, intravenously, transdermally, cutaneously.
Relief of angina pectoris. Sublingually (the tablet or capsule is kept under the tongue until completely absorbed, without swallowing), immediately after the onset of pain - 0.5-1 mg per dose. If necessary, to achieve a faster effect, the capsule should be immediately crushed with teeth; the capsule can be repeated after 30-40 minutes. In many patients with stable angina, the effect occurs with a smaller dose (1/2-1/3 tablets), therefore, if the pain goes away quickly, it is recommended to spit out the remainder of the tablet that has not had time to dissolve.
Typically, the antianginal effect appears within 0.5-2 minutes; 75% of patients note improvement within the first 3 minutes, and another 15% within 4-5 minutes. If there is no antianginal effect, another 0.5 mg of nitroglycerin should be taken during the first 5 minutes. If there is no therapeutic effect after taking 2 tablets, you should immediately call a doctor. Duration of action after sublingual administration is about 45 minutes.
For frequent attacks of angina, it is advisable to prescribe prolonged forms of nitrates. If an angina attack develops during treatment with long-acting nitrates, nitroglycerin must be taken sublingually to stop the acute attack. Tolerance to sublingual forms of nitroglycerin develops infrequently, however, if it occurs in some patients, the dose of the drug must be gradually increased, bringing it to 2-3 tablets.
To prevent angina pectoris, take it orally with water before meals. In mild cases - 1-2 tablets of 2.9 mg 2-3 times a day. In more severe cases - 1-2 tablets of 5.2 mg 2-3 times a day. The maximum daily dose is 34.8 mg. Due to the fact that the bioavailability of nitroglycerin from retard tablets is low, it is recommended, if well tolerated, to take 1-3 tablets at a time regularly 3-4 times a day or periodically, 30-40 minutes before the expected physical activity. If the therapeutic effect is insufficient, the dose can be gradually increased (but not more than 2 tablets per dose), and after the onset of a therapeutic effect, it can be reduced.
1% solution for sublingual use: relief of an attack - 1-2 drops sublingually or 2-3 drops applied to a small piece of sugar and keep it in the mouth, without swallowing, until completely absorbed.
Buccal: a plate with a selected dose of nitroglycerin is glued to the oral mucosa, usually in the upper gum area above the canines or small molars. To do this, simply press the plate with your finger against the oral mucosa for a few seconds. The action occurs almost immediately and lasts 3-4 hours or more. To prevent angina attacks, 1 mg films are used for 1-1.5 hours, and 2 mg films are used for 2-3 hours. If it is necessary to increase the flow of nitroglycerin into the blood (including during intense walking, climbing several floors), you should lick the film 2-3 times with your tongue without moving it from its place. If physical activity exceeds the period of resorption of the film, it is necessary to stick a new one on the opposite side of the gum.
Use during pregnancy and breastfeeding
Information not described.
Side effects
From the nervous system and sensory organs:
headache, dizziness, feeling of fullness in the head, weakness, restlessness, psychotic reactions, blurred vision, exacerbation of glaucoma.
From the cardiovascular system and blood (hematopoiesis, hemostasis):
flushing of the face, palpitations, hypotension, incl. orthostatic, collapse, methemoglobinemia.
From the gastrointestinal tract:
dry mouth, nausea, vomiting, diarrhea,
From the skin:
cyanosis, skin hyperemia.
Allergic reactions:
itching and burning, allergic contact dermatitis (when using transdermal forms).
Other:
hypothermia, feeling of heat, paradoxical effects - an attack of angina, ischemia up to the development of myocardial infarction and sudden death; development of tolerance.
special instructions
The drug contains dextrose (glucose), which must be taken into account when used in patients with diabetes.
In acute myocardial infarction or acute heart failure, it should be used only under the condition of careful clinical monitoring of the patient.
To prevent an increase in angina attacks, abrupt withdrawal should be avoided.
To prevent an undesirable decrease in blood pressure, the rate of drug administration should be individually and methodically correct (see above). A decrease in blood pressure can be observed not only during the period of selecting the rate of nitroglycerin administration, but also later, against the background of initially stabilized blood pressure. Therefore, blood pressure monitoring should be carried out at least 3-4 times per hour throughout the entire duration of nitroglycerin infusion.
Patients previously treated with organic nitrates (isosorbide dinitrate, isosorbide-5-mononitrate) may require a higher dose to obtain the desired hemodynamic effect.
The severity of headache while taking nitroglycerin can be reduced by reducing its dose or by simultaneously taking validol.
If blurred vision or dry mouth persists or is severe, treatment should be discontinued.
While taking nitroglycerin, a significant decrease in blood pressure and the appearance of dizziness with a sharp transition to a vertical position from a “lying” or “sitting” position are possible, as well as increased angina pectoris with a sharp decrease in blood pressure, ischemia, up to the development of myocardial infarction and sudden death (paradoxical nitrate reactions ).
Interaction
Salicylates increase the level of nitroglycerin in plasma, barbiturates accelerate metabolism. Nitroglycerin reduces the pressor effect of adrenergic agonists and the anticoagulant effect of heparin (with intravenous administration). Antihypertensive, antiadrenergic drugs, vasodilators, sildenafil citrate, calcium antagonists, tricyclic antidepressants, MAO inhibitors, ethanol, quinidine and procainamide enhance the hypotensive and systemic vasodilating effects. Methionine, N-acetylcysteine, ACE inhibitors and salicylates increase antianginal activity. Unithiol restores reduced sensitivity to nitroglycerin. Dihydroergotamine, m-anticholinergics, alpha-adrenomimetics, histamine, pituitrin, corticosteroids, stimulants of the central nervous system and autonomic ganglia, bee and snake venoms, excessive insolation reduce the vasodilatory and antianginal effects.
Overdose
Symptoms:
pronounced decrease in blood pressure (below 90 mm Hg) with orthostatic dysregulation, reflex tachycardia, headache, asthenia, dizziness, increased drowsiness, feeling of heat, nausea, vomiting may develop when using high doses (more than 20 mg/kg) - collapse, cyanosis, methemoglobinemia, dyspnea and tachypnea.
Treatment:
stop further administration. The head of the bed should be lowered and the patient's legs should be raised. As a rule, blood pressure normalizes within 15-20 minutes after stopping the administration of nitroglycerin, then administration can be continued after reselecting the infusion rate.
In case of severe hypotension and/or shock, volume replacement should be performed; To correct blood pressure, it is possible to use phenylephrine and other vasoconstrictors. The use of epinephrine (adrenaline) and similar substances is contraindicated!
Depending on the severity, the following antidotes are suggested in cases of methemoglobinemia:
1. Ascorbic acid 1 g orally or as sodium salt intravenously
2. Methylthioninium chloride (methylene blue) up to 50 ml of 1% solution i.v.
3. Oxygen therapy, hemodialysis, exchange blood transfusion.
Best before date
3 years. Do not use after the expiration date indicated on the package.
Storage conditions
In a place protected from light and out of reach of children, away from fire, at a temperature of 5°C to 25°C.