People in various situations sometimes feel chest pain that subsides over time. If this recurs regularly, you need to visit a therapist so that he can find out the cause and prescribe the correct treatment. Chest pain can have different etiologies, and without the help of a doctor it is impossible to determine whether the heart is stabbing or another organ is hurting.
Character of chest pain
The nature of chest pain differs into several types:
- pressing;
- piercing;
- aching.
The pain may be localized to a specific area or may be felt throughout the entire chest and radiate to the shoulder or arm. Aching, pressing or stabbing pain in the heart area occurs under various circumstances - when changing posture, during inhalation, with increased stress, or even at rest. In terms of duration, it can be short-term or long-term.
Heart reasons
If a person’s heart hurts when inhaling, this alarming symptom cannot be ignored. In this case, the pain can be stabbing, pressing, burning in nature, which often indicates the presence of such pathologies:
- rheumatism;
- myocardial inflammation;
- functional disorders of the cardiovascular system;
- weakening of the tone of the heart muscle during anemia.
Important! It is impossible to make a diagnosis on your own, since each of the diseases has its own causes and characteristic clinical signs, which should be considered exclusively by a doctor.
Rheumatism
Rheumatism is a disease accompanied by inflammation of the connective tissues of the body, which affects the heart, blood vessels and musculoskeletal system. Among the signs of pathology are:
- joint pain;
- pain in the heart when inhaling and at rest;
- fatigue;
- formation of rheumatoid nodes;
- rashes on the skin of a pale pink color - annular rash.
Rheumatic myocardial damage is a common consequence of infectious diseases
Rheumatism occurs against the background of damage to the body by a bacterial infection or due to the development of an allergic reaction. Treatment is carried out with the help of antibacterial agents, hormonal drugs and immunomodulators. If left untreated, the disease becomes chronic, causing heart failure and many other complications.
Myocarditis
One of the symptoms of inflammatory myocardial damage is pain in the heart area during deep inspiration, walking, physical activity, and even at rest. A patient with myocarditis is concerned about the following manifestations:
- fast fatiguability;
- excessive sweating;
- shortness of breath, headache;
- attacks of increased or, conversely, slowed heart rate.
The pathology is toxic, allergic or infectious in nature. Treatment is carried out by getting rid of the underlying disease that provoked myocardial damage.
Functional disorders of the cardiovascular system
Dysfunction of the heart and blood vessels or inconsistency of their activities in medical practice is called a functional disorder of the cardiovascular system. The condition occurs as a result of disruption of the sympathetic or parasympathetic division of the human autonomic nervous system. This occurs against a background of stress and excessive emotional stress. More often, the pathology occurs in children, adolescents and women.
Symptoms of the disease include:
- pain in the heart when inhaling and moving;
- headache;
- dizziness;
- sweating;
- emotional instability;
- chronic fatigue;
- sleep disturbance.
Dysfunction of the heart and blood vessels causes many unpleasant symptoms in humans
Therapy of the disease is carried out by improving the psychological and physiological state of the patient, which often requires the participation of a therapist, psychologist, neurologist, cardiologist and other specialists.
Heart dysfunction due to anemia
Anemia or anemia is a pathology accompanied by a violation of the qualitative composition of the blood, which often causes serious biological changes in myocardial tissue. In turn, a deficiency of certain substances entails oxygen starvation of the heart and other internal organs, which causes chest pain, apathy, irritability, loss of strength, dizziness and many other negative manifestations.
Pain due to heart disease
There are a number of heart diseases that are symptomatic of chest pain.
Compressive pain occurs as a result of manifestations of ischemic diseases. With angina pectoris, an attack of pain can last up to 20 minutes. If after this the pain does not subside, then it is probably not just angina, but a myocardial infarction. During a heart attack, pain radiates to the arm, jaw, shoulder or shoulder blade.
Aching and stabbing pain in the heart area is caused by heart diseases such as myocardial dystrophy, cardiomyopathy, pericarditis, myocarditis, and cardiosclerosis.
Symptoms of thoracic osteochondrosis
The feeling of pain in the sternum with thoracic osteochondrosis is a symptom mistakenly taken by patients for pain in the heart
. Symptoms of thoracic osteochondrosis are characterized by intensification at night. They manifest themselves especially clearly when trying to straighten your back or, on the contrary, slouch, arch your back into a dome.
The severity of symptoms of thoracic osteochondrosis directly depends on the stage of the osteochondrosis disease. At the same time, negative sensations with symptoms of thoracic osteochondrosis may manifest themselves weakly (osteophytes often grow on the surfaces of the vertebrae, where there are practically no nerve endings, and the muscle corset compensates for the load for some time).
In addition to pain in the sternum and between the shoulder blades, patients often complain of the following radicular and reflex symptoms of thoracic osteochondrosis:
- a feeling of cold, burning and tingling in the chest, at the base of the neck, in the abdomen;
- muscle tension (difficulty relaxing your back);
- a feeling of pain in the sternum (a symptom of thoracic osteochondrosis, which is one of the first to appear);
- increased heart rate, feeling of pulsation in the chest;
- a feeling of “pins and needles” inside the chest, which is often accompanied by causeless anxiety or increases with stress;
- numbness of soft tissues (skin and muscles) near the spine, in the shoulders, especially noticeable when pressed or in contact with hot and cold surfaces;
- with thoracic osteochondrosis it is difficult to breathe;
- feeling of coldness in the hands and feet, pale or bluish skin on the hands;
- weakness, inhibition of reflex reactions in the affected area;
- disturbances in the functioning of the digestive organs, colic, stool disorders;
- the appearance of areas of skin with obvious nutritional disorders (peeling, pallor, thinning or, conversely, thickening of the skin);
- feeling of a lump in the chest, discomfort when swallowing large pieces of food;
- characteristic cough with thoracic osteochondrosis;
- digestive symptoms (dyspepsia, loss of appetite, nausea, heartburn, bloating);
- increased fatigue, feeling very tired in the morning (“broken” state);
- change in gait (usually stooping, unsteadiness);
- intercostal neuralgia.
The symptoms of thoracic osteochondrosis can feel like they are a stomach or intestinal ulcer, angina pectoris, gastritis or a heart attack. Sometimes it is mistaken for renal or cardiac colic, cholecystitis or pancreatitis. Indeed: advanced thoracic osteochondrosis can cause malfunctions in the gallbladder (for example, sediment formation) and intestines, and dysfunction of the heart vessels.
The specificity of the symptoms of cervical osteochondrosis depends on the location of the problem:
- 1st-2nd thoracic vertebrae
- pain radiates to the collarbone, armpit, and can reach the shoulders; - 3-6th vertebrae
- patients are bothered by girdling pain above the chest, which is similar to pain in the heart or mammary glands; - 7-8th vertebrae
- pain in the solar plexus, which imitates diseases of the internal organs (stomach, liver, gall bladder, pancreas). There is also inhibition of the epigastric reflex (contraction of the abdominal muscles when passing the instrument along the line of the lower rib); - 9-10th vertebrae
- here osteochondrosis can cause sharp pain in the abdomen and under the ribs, inhibit the mesogastric reflex (when a tool draws a horizontal line at the level of the navel); - 11-12th vertebrae
- can initiate groin pain, diseases of the internal genital organs and intestines. Reduces the hypogastric response (by drawing a line in the lower abdomen parallel to the inguinal fold).
Difficulty breathing
During physical activity (for example, climbing a couple of floors of stairs), patients find it difficult to breathe. With thoracic osteochondrosis, severe shortness of breath is observed. Patients often describe this sensation as “breathless.” Similar symptoms can be observed during sleep: in an unsuccessful position, patients dream of lack of air, their ears may become blocked (a strong pulsation can be heard), and severe chest spasms occur.
Often the feeling that it is hard to breathe with thoracic osteochondrosis is accompanied by girdle pain in the back and ribs, as well as subcostal pain.
Increased heart rate
Even after light exertion, which previously went unnoticed, patients complain of increased heart rate, feeling as if the heart is trying to jump out of the chest. At first, increased heart rate may be caused by spastic contractions of the muscles and chest or a violation of tissue trophism, but over time, this dangerous symptom can actually outgrow angina pectoris, coronary heart disease and even lead to a heart attack.
In addition to increased heart rate, patients often note an accompanying feeling of panic, fear of death, or increased background anxiety. In some cases, against the background of thoracic osteochondrosis, real panic attacks can be observed.
Chest pain
The most telling symptom of thoracic osteochondrosis is a feeling of pain in the sternum
.
These include sharp shooting pains and a feeling of pressure in the chest, as well as intercostal pain when walking. Chest pain tends to intensify after a long stay in one position, hypothermia, turning the body and bending (especially with a turn), raising the arms. Carrying heavy objects, playing sports, taking deep breaths, and sleeping still can also increase pain. It should be remembered that due to the low mobility of the thoracic spine, osteochondrosis in this part of the back is characterized by dull, aching, pressing and throbbing pain. Acute, prolonged pain with thoracic osteochondrosis is very rare, which is why patients tend to ignore the pathology for a long time
.
Vertebral pain
With osteochondrosis of the spine, it is customary to divide into dorsago and dorsalgia.
Dorsago
is a spontaneous shooting pain that, as a rule, does not last long and goes away with a change in position.
Dorsago is usually caused by accidental root pinching. Dorsalgia
is long-lasting (about 2-3 weeks) and is associated with permanent disruption of blood circulation or nerve conduction. They make themselves felt by burning, stinging pain.
The pain intensifies when coughing and can be mistaken by patients for a spinal hernia. However, with osteochondrosis of the thoracic region, hernias are extremely rare. Don't write off the main symptom
(feeling of pain in the sternum with thoracic osteochondrosis)
to a displacement of the vertebra - its probability is extremely low in comparison with degenerative-dystrophic changes
!
Cough with thoracic osteochondrosis
Cough with thoracic osteochondrosis is often observed in people who lead a sedentary lifestyle, and their work duties involve prolonged sitting (office workers, operators, drivers). Maintaining this posture, which is difficult for the human spine, causes chronic muscle strain, spasms and tightness. Spasticity
is both a cause and a consequence of the fact that the cervical and thoraco-girdle area suffers from insufficient movement. At night, in positions that compress the spine, spasms and irritation of the spinal roots only intensify, causing severe coughing. If the upper thoracic vertebrae are affected, a cough due to thoracic osteochondrosis may be accompanied by pain in the esophagus, a feeling as if something is stuck in the chest.
During coughing attacks with thoracic osteochondrosis, it becomes painful for patients to breathe; It becomes difficult to take a deep breath.
Chest pain due to gastrointestinal and respiratory diseases
When an esophageal ulcer worsens, severe pain occurs in the chest, as a result of which in some cases the person may lose consciousness. The pain occurs when eating, and is similar in nature to the symptoms of angina pectoris; it seems as if the heart is stabbing. The same pain occurs with cancerous tumors, Mallory-Weiss syndrome (rupture of the esophagus) and also as a result of chemical burns of the esophagus.
Lung diseases, such as pneumonia, bronchitis, pleurisy, tuberculosis and silicosis, are manifested by aching pain and heaviness in the chest. Symptoms that differ from heart disease are cough, which may include shortness of breath and respiratory failure. As a result of shortness of breath, many people experience heart palpitations.
Chest pain due to sprains, intercostal neuralgia and injuries
With intercostal neuralgia, which manifests itself as a result of muscle spasm, the nerve roots are compressed, and a sharp pain occurs in the chest, radiating to the back.
Chest pain can also be caused by damage to the pectoral or back muscles - sprains, tumors (rhabdomyoma), inflammation (myositis).
Pain from bruises, fractures or cracked ribs can also be mistaken for heart pain. However, by the location of the source of pain, it can be determined that it is not the heart that is hurting.
If you have chest pain or heart pain, contact our clinic. Experienced doctors will make the correct diagnosis and prescribe a course of treatment.
Sharp pain in the heart
Unpleasant sensations in the chest area may indicate pathologies of the cardiovascular system and gastrointestinal tract. In this case, sharp pain in the heart can also be explained by heart disease or a disorder of other organs. To identify the exact cause of such a symptom, a thorough diagnosis may be required, including instrumental and laboratory research methods.
Features of pain
The characteristics of pain are an important indicator, since symptoms change with different pathologies. Thus, with coronary artery disease, sharp pain in the heart can disappear without treatment within 15-20 minutes, and with a heart attack, sharp stabbing pain in the heart only intensifies over time. It is also important to identify the type of pain sensation. It can be stabbing, squeezing, aching or cutting pain.
It is also important to consider the distribution of pain. Doctors often say that localized pain in the chest area or solar plexus is often associated with gastrointestinal diseases, and not with the heart. An alarming signal is a sharp pain in the heart area, gradually spreading to the upper limbs, back, neck and lower jaw. These are common signs of myocardial infarction.
8
24/7
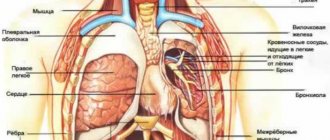
Function of the cardiovascular system
The key to understanding the causes of chest discomfort is the physiology of the heart and blood vessels. Thus, the heart is a powerful muscular organ, the continuous operation of which provides all tissues of the body with nutrients and oxygen. The constant frequency and strength of the heartbeat, regulated by internal and external structures, maintains hemodynamic constants, including blood pressure and blood flow patterns. The myocardium and membranes of the heart contain a large number of receptors associated with the nervous system. Painful sensations can appear due to injuries, hypoxia of muscle cells, inflammation and other ailments.
We should not forget that the heart is close to other anatomical structures. These are primarily the esophagus, lungs, spine and celiac plexus. Disease in other organs can also cause symptoms similar to those of a heart disorder. For example, a sharp pain in the heart when inhaling may well be associated with air entering the pleural cavity or neuralgia. Without a thorough diagnosis, it is impossible to determine the exact cause of pain.
Possible causes of the symptom
The search for the source of pain should be aimed at diagnosing all organs of the chest. If characteristic signs of a heart attack, internal bleeding or other acute pathology appear, emergency medical attention may be required. It is also important to immediately exclude pulmonary, neurological or gastrointestinal pathology.
Diseases of the heart and blood vessels that cause severe pain in the heart:
- Ischemia of cardiac muscle tissue. If there is insufficient blood supply to the myocardium, severe complications can occur. The condition may be associated with atherosclerosis of the coronary arteries or impaired vascular tone. Coronary artery disease often manifests itself as severe chest pain called angina. It is important to be able to distinguish angina from signs of a heart attack or gastroesophageal reflux.
- Myocardial infarction is partial destruction of the muscular lining of the heart as a result of prolonged hypoxia of cardiomyocytes. This is the most dangerous cardiovascular disease. The sharp pain in the heart that occurs during a heart attack is in many ways similar to an angina attack.
- Aortic aneurysm is the formation of a pathological pocket in the wall of the artery. In this case, a significant expansion of the aorta occurs. Aneurysms are dangerous due to possible rupture of the wall of the affected vessel and extensive bleeding.
- Pericarditis is an inflammatory pathology of the membrane surrounding the heart (pericardium). Fluid may gradually accumulate in the pericardial cavity, interfering with the heartbeat. In this case, sharp pain in the heart occurs due to compression of the myocardium and disruption of the blood supply to the organ.
- Myocarditis is inflammation of the muscular lining of the heart. Pathology may have a viral or bacterial etiology.
- Myocardial contraction rhythm disorder. Arrhythmia is characterized by too frequent, infrequent or chaotic heartbeats. Pain in such a disease is often caused by impaired blood supply to organs.
- Damage to the heart and blood vessels due to chest trauma. Often, patients injured in accidents have no visible signs of injury, but doctors later discover internal bleeding.
- Aortic dissection is a rupture of the wall of a large artery arising from the left ventricle.
- Consequences of heart surgery. Thus, damage to large bundles and nodes of the conduction system can cause rhythm disturbances.
8
24/7
Possible causes not related to diseases of the cardiovascular system:
- Gastroesophageal reflux is the release of acidic stomach contents into the esophagus. Substernal pain may occur.
- Gallstones that prevent the release of secretions into the small intestine.
- Inflammatory diseases of the esophagus.
- Diseases of the pancreas, including acute and chronic pancreatitis.
- Pneumonia is an infectious disease of the lung tissue.
- Pneumothorax is the entry of air into the pleural cavity with subsequent respiratory failure.
- Blockage of the pulmonary artery and general hemodynamic disturbance.
- Obstructive pulmonary disease.
- Neuralgia.
- Fracture of the ribs or sternum.
- Anxiety disorder.
The abundance of possible causes makes initial diagnosis difficult. Sharp pain in the heart can be caused by even minor stress.
Other symptoms and signs
Sharp, severe heart pain is rarely the only symptom, so differential diagnosis may require identifying additional symptoms and signs. First of all, it is important to evaluate objective signs of the cardiovascular system, including:
- Blood pressure.
- Pulse rate.
- Heartbeat sounds on auscultation.
In addition to discomfort in the chest, the following signs may be detected:
- Nausea and vomiting.
- Dizziness.
- Loss of consciousness.
- Abdominal pain.
- An unpleasant taste in the mouth and a burning sensation in the throat.
- Spread of pain to the upper extremities, lower back, lower jaw and neck.
- Breathing disorders, shortness of breath.
- The appearance of cold sweat.
- Panic attack.
- Muscle weakness.
- Stupor or stupor.
If the pain spreads to the back, limbs and jaw, you should immediately consult a doctor. Also, patients with coronary heart disease should pay attention to the nature and duration of angina. If the attack lasts longer than 20 minutes and nitroglycerin does not help, you should also urgently seek medical help.
Diagnostics
Sharp pain in the heart, the causes of which may be associated with different organs of the chest, often requires a comprehensive diagnosis. The patient can seek advice from a therapist, cardiologist or neurologist. During the appointment, the doctor will conduct a physical examination to assess objective signs of the disease, ask about complaints and study the medical history.
Additional diagnostics:
- Electrocardiography – registration of the bioelectrical activity of the heart. To do this, special sensors are placed on the patient’s body connected to a cardiogram recording device. Based on the test results, one can judge the presence of a structural pathology that prevents the normal propagation of an impulse in the myocardium.
- Echocardiography is the main imaging method in cardiology. The doctor uses a transducer that sends high-frequency sound waves into the heart to produce an image. Monitoring the heart's performance on a monitor in real time allows you to detect the pathological area and assess the degree of pumping dysfunction.
- Coronary angiography – visualization of blood vessels. As a rule, this method is used to diagnose coronary artery disease, heart attack and atherosclerosis. Before taking the image, the doctor injects a contrast agent intravenously to improve the accuracy of the study. Based on the results of coronary angiography, one can judge the cause and degree of narrowing of the vessel.
- Blood tests for signs of infection, hormones, electrolytes, and heart attack indicator enzymes.
- Bicycle ergometry - obtaining a cardiogram during frequent heart contractions. This test is most often used to diagnose hidden arrhythmia that occurs against the background of significant stress.
- Holter study – recording of a cardiogram on an electronic device of a portable device within 24-48 hours. Before the study, the patient is instructed to keep a diary of well-being to clarify the time of occurrence of heart pain.
- Cardiac biopsy – removal of a section of heart tissue followed by histological examination.
- Computed tomography and magnetic resonance imaging are methods for obtaining high-resolution images of the heart and blood vessels. The images are often used to plan surgery.
- Endoscopic examination of the esophagus, stomach and intestines to look for signs of injury, inflammation or infection
A person with pain in the heart area may also need to consult a psychotherapist if all objective studies refute the pathology of the heart and blood vessels. Seeing a doctor early increases your chances of effective treatment, so don’t delay making an appointment.
8
24/7