Temporal (giant cell) arteritis is a chronic inflammatory process that occurs as a result of a malfunction of one’s own immune system, affecting various arteries. Another name for this disease is Horton's disease. It received this name thanks to the doctor who described the pathology in detail.
The exact cause of temporal arteritis is currently unknown. But there is an opinion that its appearance is facilitated by the aging of the body. The fact is that with age, the walls of the temporal and ophthalmic arteries and veins become less elastic, which is why immune inflammation occurs. Since this disease affects the visual system, in rare cases, lack of treatment can cause complete blindness.
Also, according to some experts, Horton's disease has some genetic predisposition. Most often women are susceptible to it.
The disease has two forms - primary and secondary. In primary temporal arteritis, it occurs independently. This form develops due to age-related changes, usually in people over 50-60 years old. The secondary form indicates the occurrence of another disease, which is a catalyst for inflammation. Most often this concerns infectious diseases in a severe stage. The most dangerous among such infections are Staphylococcus aureus and the hepatitis virus.
Causes
Not a single theory of the origin of the disease has been reliably confirmed.
Presumably, the infectious factor plays an important role in its development. There is often a natural connection between the occurrence of arteritis and previous influenza and group B hepatitis. The genetic programming of pathology also has its supporters. Cases of this rather rare disease have been observed in close relatives and identical twins. The leading role in the formation of inflammation of the vascular wall belongs to immunological disorders, and this is recognized by adherents of all etiological concepts. With temporal arteritis, the immune system reacts inadequately to its own tissues - the process proceeds as an autoimmune one.
Types of temporal arteritis
Basically, in medicine there are two types of disease:
- Primary.
It mainly develops in older people as a separate independent disease. Granulomas in this case are not infectious in nature. - Secondary.
Such arteritis is a consequence of infectious or viral diseases, which at one time were in a severe or advanced stage.
If we look at it from a developmental perspective, doctors highlight:
- segmental arteritis
– affects individual parts of the body; - focal arteritis
is a holistic mass disorder of vascular functionality.
Symptoms
The disease has no characteristic onset. Several options are possible: acute, subacute, but more often with a long period of precursors, which can last several weeks or more than one month.
The set of symptoms preceding the height of the disease and united under the general name polymyalgia rheumatica includes the following manifestations:
• general malaise;
• slight increase in body temperature within 37.2–37.5°C;
• excessive sweating, especially at night;
• aching joints;
• pain in the muscles;
• sleep disorders;
• weight loss.
Later, vascular disorders come to the fore; their nature and severity depend on the location and degree of damage to the artery. More than half of patients suffer from vision impairment. Patients note:
• headache of varying intensity, often sudden, in various areas (temporal, frontal, parietal, less often - occipital);
• hyperesthesia (increased sensitivity) of the scalp, making it difficult to comb and wear a hat;
• transient pain and numbness in the tongue and lower jaw, which intensifies when talking and chewing;
• painful, stringy compaction along the inflamed artery;
• visual impairment (decreased visual acuity, diplopia (double image), blindness);
• neurological, mental disorders.
When the aorta, coronary, renal, and mesenteric arteries are involved in the pathological process, which happens in severe untreated variants of the disease, the development of aneurysm, angina pectoris and heart attack, impaired blood supply and kidney and intestinal function are possible.
Reliability of ultrasound
The use of ultrasound is increasingly recommended as a first-line diagnostic modality in patients with suspected GCA and can replace temporal artery biopsy (TAB) in most cases. Conversely, questions have been raised regarding the diagnostic performance and reliability of ultrasound and ascertaining the overall clinical utility of ultrasound in GCA.
To address these issues, the OMERACT initiative on ultrasound in videoconferencing was created in 2014; it includes members from Europe and the USA. The OMERACT initiative is designed to achieve consensus on common, consistent definitions that can be used in future clinical trials and to test the reliability of these definitions for image and video interpretation, and for imaging and interpretation in patients. The basis for these determinations was a systematic review of publications on ultrasound and other imaging modalities for the diagnosis of VCS using the Ovid MEDLINE, EMBASE and Cochrane databases up to March 2021. Full research articles of prospective studies involving more than 20 patients with suspected (diagnostic studies) or established (follow-up studies) primary VCS. Case–control studies and studies using continuous wave Doppler and M-mode ultrasound to examine vessel wall pulsatility were excluded because they were not considered relevant to clinical practice. A meta-analysis was also conducted to summarize the data. This work also forms the basis of the EULAR recommendations for imaging in VCS. The EULAR recommendations are expected to be published soon.
Studies that met the selection criteria for the systematic literature review included ultrasound, MRI, CT, and PET; however, the majority of selected studies examined ultrasound. The overall sensitivity and specificity of temporal artery ultrasound were 77% and 96% compared with clinical diagnosis of GCA, with likelihood ratios of 19 and 0.2 for positive and negative ultrasound, respectively. Three older meta-analyses found specificities of 83%, 91%, and 94% for the halo symptom compared with clinical diagnosis. The first meta-analysis described a sensitivity of 55% for the halo symptom, which increased to 87% when accounting for stenosis and occlusion. Another meta-analysis showed a sensitivity of 68% and 75% for the halo symptom. Detection of a bilateral halo sign increased specificity to 100%. In more recent studies, sensitivity has been higher due to improved technology and growing experience; this improvement is reflected in the most recent meta-analysis. A recently published study of 451 patients with suspected GCA, of whom 256 patients had a final diagnosis of GCA, showed a sensitivity of 91.6% and a specificity of 95.8% for ultrasound compared with the final clinical diagnosis. Another recent study (TABUL) examined the diagnostic accuracy and cost-effectiveness of US compared with BVA. In this multicenter study, the sensitivity of ultrasound compared with clinical diagnosis at 6 months was unexpectedly low (54%); however, it was higher than the sensitivity of BVA (39%). It is difficult to determine the gold standard for diagnosing GCA for testing any new diagnostic modality such as ultrasound and other imaging modalities. Despite this caveat, it is clear that BVA is less sensitive than ultrasound in most studies, especially because BVA evaluates only a limited anatomical region in systemic disease.
How reliable is ultrasound? In radiology, it is common practice to evaluate the reliability of image interpretation, but not to simultaneously evaluate image acquisition and interpretation. Although scientific evidence is lacking, ultrasound is highly operator dependent. Solving this problem requires data and interpretation to obtain images. One Spanish study showed very high reliability of image and video interpretation of temporal artery ultrasound. For all scenarios, k-values were >0.8, suggesting almost perfect agreement. In another study, interoperator agreement in the diagnosis of GCA between two sonographers at the same institution assessing the symptom of temporal artery compression was excellent, with the two sonographers disagreeing in only 1 of 60 patients. However, these data need to be confirmed by large-scale international studies.
In an online test of the reliability of images and videos of the temporal and axillary arteries of GCA patients and controls following the strict ultrasound guidelines associated with OMERACT, the OMERACT ultrasound group also achieved k-values >0.8 for intra- and inter-operator agreement for halo symptoms and compression. The TABUL study used even stricter rules when assessing the reliability of video data from 12 sonographers randomly selected from the study database, regardless of their quality. Reliability was equal to that of the 14 pathologists who described the BVA specimens, with intraclass correlation coefficients of 0.61 and 0.62, respectively. Sonographers in the TABUL study were less experienced than sonographers in the OMERACT study. Both studies show that ultrasound images and videos can reliably confirm the diagnosis of GCA. This allows the use of ultrasound as an inclusion criterion for future studies of GCA, provided that stored ultrasound videos are available for subsequent review.
Reliability has also been tested according to OMERACT guidelines in studies of patients in several other diseases such as RA and gout. This test is difficult to perform in patients with GCA because GCA responds quickly to treatment. However, a recent study was conducted with very good reliability for the overall diagnosis of GCA and moderate to good reliability for the detection of vasculitis in the relevant anatomical segments.
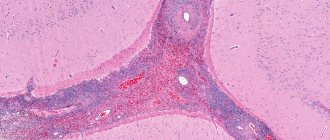
Diagnostics
The diagnosis of arteritis can be established by performing a histological examination of a section of the superficial temporal artery obtained by biopsy. The sample collection is carried out under local anesthesia and is not difficult. The detection of granulomatous inflammation of the vascular wall with the presence of giant cells is indisputable evidence of this pathology.
But histologists are able to identify typical changes only in half of the cases. The fragmentary nature of the lesion does not always allow for successful selection of the segment for biopsy. However, a negative result does not mean the absence of the disease, since the main criterion for diagnosing Horton’s disease is the totality of clinical manifestations.
Criteria have been formulated and generally accepted to recognize temporal arteritis. The diagnosis is reliable if three or more of the following factors are present:
• age over 50 years;
• headaches with severe intensity;
• vision problems;
• presence of complaints characteristic of polymyalgia rheumatica;
• decrease in the number of red blood cells and hemoglobin level in the blood, increase in ESR.
Sphygmography, rheovasography, and Dopplerography of the affected arteries are of auxiliary value for differential diagnosis. For the same purpose, the presence of C-reactive protein and the level of sialic acid and fibrinogen in the blood are determined.
Technical requirements
Modern, high-resolution linear Doppler probes should be used, especially for the study of the temporal arteries. Ultrasound resolution increases with increasing frequency, and tissue penetration increases with lower frequencies. Probes with frequencies >=15 MHz should also be used to examine the temporal arteries for mild wall thickening. Transducers with frequencies >20 MHz are increasingly available and allow clear visualization of normal temporal artery IMT.
Treatment
At the moment, there are two directions in the treatment of temporal arteritis: therapeutic and surgical . Surgical methods are resorted to in the event of the development of complications such as aortic aneurysm and thrombosis of blood vessels, especially those supplying blood to the eyeball.
The basis of treatment for the disease, without which it is impossible to achieve positive results, is the prescription of steroid hormones (prednisolone). There is no alternative to glucocorticoids. They are prescribed as early as possible and taken for a long time. Doses and regimen are selected individually, under constant laboratory monitoring of clinical and biochemical blood parameters. A combination of hormones and drugs that suppress immune responses is possible. Symptomatic treatment is also carried out using anticoagulants, agents that improve microcirculation, and vitamins.
Prevention
Due to the fact that the causes of the disease are not fully understood, doctors cannot give practical, effective measures for prevention. Despite this, there is a clear connection with the transmission of infectious diseases, so a person should carefully monitor the state of his immune system.
- Normalize your daily routine, go to bed on time, take breaks during heavy and active exercise.
- Watch your diet, do not eat junk food, drink enough water per day.
- Take vitamins, eat fruits and foods that are healthy for the body.
- If you have the slightest signs or suspicion of temporal arteritis, consult a doctor immediately.
- Complete abandonment of bad habits that affect the functioning and tone of blood vessels.
- Practice moderate physical activity in the form of gymnastics or other simple exercises.
- It's great if you toughen up in the morning. A morning contrast shower has a positive effect not only on your health, but also on your mood.
- Ventilate the room before going to bed.
Forecast
Temporal arteritis is a serious disease. If not recognized in a timely manner and treated inadequately, the pathology poses a threat to the health and life of the patient. A timely diagnosis and compliance with doctors’ recommendations avoid complications and make the prognosis favorable.
In our department of vascular surgery, a full examination, qualified interpretation of the results obtained and professional implementation of all types of treatment measures are possible.
Prognosis, possible complications
If treatment is carried out at the initial stage of the disease, the prognosis is favorable. Steroid therapy will help block arteritis and get rid of negative symptoms. Laboratory parameters gradually normalize, the condition of the vascular walls improves, and blood flow is restored.
Since the disease is autoimmune in nature, it cannot be completely cured. Without treatment, complications are possible:
- blurred vision, blindness;
- the disease enters the chronic stage;
- arterial thrombosis;
- angina pectoris;
- formation of ischemic areas in the brain;
- formation of necrotic areas;
- neurological and mental disorders.
Important! Properly selected therapy will help eliminate the disease in time, eliminating the risk of heart attack, blindness, and stroke.