© Author: Sazykina Oksana Yuryevna, cardiologist, especially for SosudInfo.ru (about the authors)
Sudden cardiac death in recent years is not as rare as it used to be, and has become more common even in young patients. This condition can occur anywhere - on the street, in public transport, at sporting events, etc. In this regard, any person, and not only a medical worker, should know how to correctly and timely provide emergency assistance to the victim. This is especially true for such techniques as precordial stroke. Of course, when carrying out such a strike, there are rules, which will be discussed below.
So, a precordial stroke is a method of physical impact on the chest of a patient who has suffered cardiac arrest. Such an effect can translate physical vibrations of the anterior chest wall and the wall of the heart into electrical excitation of the fibers of the heart muscle, since the heart tissue has the property of electrical excitability, as a result of which its mechanical irritation can provide an electrical impulse response. In other words, the mechanical effect on the heart area is a kind of mechanical pacemaker, thanks to which the normal cardiac cycle can start again. However, a number of authors are inclined to believe that such an effect is not enough to produce a full-fledged electrical systole, capable of ensuring adequate ejection of blood into the aorta, and, consequently, ensuring blood flow to the brain. There has been a lot of debate about this effect on the heart in the medical literature, and yet at the present time:
A precordial shock is considered an effective resuscitation aid, but only if the patient actually has a cardiac arrest, and the shock was carried out in the first 30-40 seconds after that.
When is it necessary to perform a precordial stroke?
The indication for carrying out this resuscitation aid when providing first aid is the absence of an independent heartbeat in the patient, which is caused by ventricular fibrillation and/or asystole (cardiac arrest) due to other rhythm disturbances. Clinically, asystole, which caused clinical death, is accompanied by such signs as:
- Loss of consciousness
- Absence of pulse in the carotid and femoral arteries,
- Dilated pupils with lack of reaction to light,
- Lack of independent breathing movements,
- The presence of a blue tint on the skin of the face, neck, and hands.
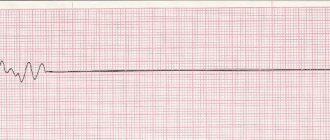
If the doctor has the ability to conduct an ECG or cardioscopy using a monitor on a defibrillator, ventricular fibrillation, electromechanical dissociation of the heart and asystole can be reliably detected.
The algorithm for diagnosing cardiac arrest is as follows:
- If a person falls and loses consciousness, you should call out to him and shake him by the shoulder. It is unacceptable to hit a person on the cheeks; you can sprinkle water on your face.
- If there is no reaction, feel the pulse fluctuations of the carotid artery (at the angle of the lower jaw), assess the presence of independent respiratory movements - see if there is an excursion of the chest, listen to the sound of exhaled air with your ear or feel the exhaled air with your cheek (the “look, listen, feel” algorithm ).
- In the absence of pulse and respiratory movements, immediately begin performing a precordial stroke with further indirect cardiac massage and artificial ventilation using artificial respiration.
The patient will be saved by prompt and correct actions
The victim is placed on a flat and hard surface. The man lies on his back. The cardiologist is inclined to prohibit performing the shock on a bed or soft surface. It absorbs kinetic energy. The procedure loses its effectiveness. The further procedure is as follows:
- the pulse is checked in the carotid and femoral arteries;
- absence of a pulse is a reason to immediately call an ambulance;
- An assistant calls the doctors, and the person begins resuscitation;
- at the point where the blow will be struck, they are freed from clothing;
- everything is removed from the victim’s clothing pockets - small and not so small objects will damage the skin during the manipulation;
- a right-handed person places the index and middle finger of his left hand in the solar plexus area on the chest;
- the fingers are placed at the so-called point of convergence of the ribs (solar plexus) - the more accurately the point is found, the less the risk of violating the integrity of the xiphoid process;
- a left-handed person repeats what was described above with only one difference - they use the fingers of the right hand;
- the second hand, which will receive the impact (blow), is clenched into a fist;
- the cardiologist is inclined to prohibit applying the impact with the edge of the palm;
- the clenched fist is raised above the point where the blow will be struck by 25 cm;
- the person who carries out resuscitation measures sits on the side of the victim;
- the hand clenched into a fist is located above the heart area and parallel to the body;
- the elbow of the hand clenched into a fist “looks” towards the victim’s navel;
- deliver a sharp blow at equal intervals no more than 2 times;
- after each sudden impact, check the pulse in the carotid and femoral arteries.
As soon as the pulse is recorded, a cardiac massage is performed. It is performed before the ambulance arrives. Correct implementation of recommendations increases a person’s chances of survival. In percentage terms, the situation looks like this. Of every 10 victims who were hit, at least 6-7 survived.
On a note!
A precordial blow is administered to children under 10 years of age with great caution - this kind of resuscitation is possible only after a detailed calculation of the force of impact. There shouldn't be any mistakes. There is a high risk of damaging the child's internal organs.
Precordial stroke is a method of restoring heart rhythm in the event of clinical death. The essence of the manipulation is reduced to a sharp effect on the chest. If the procedure is carried out within the first 45 seconds after the onset of clinical death, there is a high probability of resuscitating the victim. Resorting to a blow is allowed in the case when the performer masters the technique perfectly. Mistakes are not allowed.
7
When should you not apply a precordial blow?
This resuscitation aid is strictly not applied in the presence of a pulse in the carotid artery and in the presence of independent respiratory movements. This is fraught with cardiac arrest in a person who has simply lost consciousness or is in a coma, as well as in a patient with convulsive syndrome. That is, the absence of consciousness in a patient with a normal heart rhythm can be mistakenly regarded as clinical death, as a result of which a precordial blow can cause irreparable harm to the patient.
If the victim has open injuries to the chest (open gaping wounds with massive bleeding, prolapse of chest organs into the lumen of the wound), and it is also possible to visually determine rib fractures (deformation of the ribs, protruding parts of the ribs), performing a precordial blow is pointless. In this case, you should wait for doctors or rescuers to arrive.
Thus, the only contraindication for performing a precordial blow with an intact chest frame without visible damage is the presence of a pulse in the carotid or femoral arteries, as well as the presence of an independent heart rhythm on the cardiogram or on the cardioscope of the defibrillator.
Regarding pediatric patients, it should be noted that performing a precordial stroke is strictly contraindicated in children under 7 years of age due to the high likelihood of damage to internal organs. This category of victims immediately begins performing indirect cardiac massage.
What is the essence of the method?
The mechanism of precordial shock is chest compression. With sharp compression, the contractile activity of the ventricles of the heart is provoked, their blood filling and depolarization - an artificial start of the rhythm.
The method is effective at the first symptoms of cardiac arrest for up to 40-60 seconds, then compression strokes do not have the desired effect due to the progression of fibrillation, low blood discharge, and cardiac arrest.
When performing the procedure, a mechanically generated impulse occurs in the electrically excitable heart muscle from a sharp compression of the skeletal muscles. The heart muscles are anatomically built in such a way that they react with automatic excitation to an external trigger - a compression push of the chest.
An electrical impulse response most often occurs when mechanical and electrical effects are combined - performing a sequential complex of precordial shock and defibrillation electrodes on the patient’s body.
Technique for performing a precordial stroke
So, the precordial blow is applied correctly in a certain way. After a person has fallen and lost consciousness, the person providing assistance (hereinafter referred to as the resuscitator) must perform a series of sequential actions within 30-60 seconds:
- Turn the patient onto his back , placing him on a hard, flat surface (floor, ground). In no case should resuscitation be performed on a soft bed, since the chest will be “pressed” into the soft surface, and the desired effect from mechanical shaking of the chest wall will not be achieved.
- Check the pulse in the carotid artery (at the angle of the lower jaw) or in the femoral artery (in the groin).
- If there is no pulse, you should give a voice command to nearby people in order to urgently call an ambulance or rescuers. It is unacceptable to waste precious time searching for a phone yourself, as seconds count. If there are no other people nearby, you should loudly call passers-by for help.
- Simultaneously with the call for help, it is necessary to expose the victim's chest . It is unacceptable to perform a precordial blow on a person wearing a shirt, since the resuscitator may not notice small metal objects in the sternum area (pectoral cross, metal jewelry, coins, etc.). In the latter case, traumatic injury to the chest is more likely.
- After exposing the chest, the resuscitator places the index and middle fingers of the non-working hand (left for right-handed people, right for left-handed people) on the lowest part of the sternum directly above the epigastric region, that is, where the ribs meet the sternum. It is here that the most vulnerable part of the sternum to traumatic injury is located - the xiphoid process . Thus, the resuscitator covers it with two fingers at the moment of impact.
- Now you need to raise your working hand, clenched into a fist, to a height of 20-30 cm above the victim’s sternum. The correct position of the resuscitator in this case is that the resuscitator stands to the side of the victim, facing him. The working arm is raised above the patient’s chest, with the forearm directed parallel to the victim’s sternum (the resuscitator’s elbow is directed towards the victim’s stomach). When the forearm is positioned transversely (the elbow is directed towards the resuscitator), damage to the sternum is inevitable. With considerable force, one or two short blows should be made twice to the area of the uncovered part of the sternum.
You should immediately check the pulse in the major arteries. In any case, both in the presence of a pulse and in its absence, indirect cardiac massage immediately begins at a rhythm of 60-100 compressions per minute.- Precordial shock is no longer performed, but cardiac massage is performed until rescuers arrive or no less than 30 minutes from the start of resuscitation.
Figure: Performing a precordial beat
If cardiac arrest occurs in a medical facility, there is no point in wasting time looking for a defibrillator, since it is necessary to immediately begin delivering a precordial shock. If a defibrillator is at hand, for example, when cardiac arrest occurred in the intensive care unit, the resuscitator should immediately determine the type of asystole using a cardioscope and begin defibrillation using electrical pulse therapy.
Physiological aspect
The precordial blow is used when providing first aid to the victim. Sharp compression of the chest triggers the contractile reflex. The ventricles of the heart fill with blood. The rhythm is restored. A sharp compression of the chest forms an impulse. Directed mechanical energy provokes excitation at the nerve endings.
On a note!
The shock is carried out within the first 65 seconds after the onset of sudden cardiac arrest. After 1.5-2 minutes of clinical death, the method is useless.
Indications and contraindications
Cardiologists have identified a list of indications for which a precordial stroke is performed.
| Indications | Contraindications |
| Loss of consciousness - the patient cannot feel a pulse | A “thread-like” pulse is recorded in one of the arteries of the victim. |
| The onset of sudden clinical death. Its duration does not exceed 45 seconds | Presence of breathing movements |
| Development of sudden ventricular arrhythmia | Convulsive muscle contractions |
| – | Presence of injury in the chest area |
| – | Age up to 10 years |
| – | Body weight up to 15 kg |
After 5 minutes of resuscitation measures, the physician makes a conclusion about the occurrence of death. Unfortunately, surgery does not always restore the heart rhythm. Doctors recommend stopping all attempts to revive the patient if several signs are present. The first is that the eyes do not respond to the influence of a light stimulus. The second sign is that the epidermis changes color.
Precautions and complications
Cardiologists allow manipulation to be carried out by those who know how to strike correctly. The procedure is considered traumatic. Hasty actions in the chest area will provoke injuries:
- rib fracture;
- internal bleeding;
- violation of the integrity of the lung tissue;
- pleural rupture;
- respiratory arrest;
- damage to internal organs and so on.
It is up to everyone to minimize the likelihood of complications. It is enough to remember the precautions. Cardiologists prohibit honing their skills on healthy people. There is a high risk of causing irreversible changes in the functioning of the cardiovascular system. The blow is allowed to be delivered in the presence of cardiac arrest. Other recommendations are as follows:
- efficiency and accuracy - the blow is delivered within the first 45 seconds after the onset of clinical death;
- before starting the manipulation, feel the pulse at 2-3 points;
- The patient's chest is freed from clothing.
Increased caution is required when acting on the xiphoid process, a narrow and short element of the sternum. Do not use excessive force when striking. Excessive exposure will cause damage to the appendix or disruption of liver tissue. Pathological changes in a vital organ will not keep you waiting.
On a note!
Precordial stroke is a controversial, not prohibited, method. Cardiologists continue to debate the advisability of its use. The effectiveness of the manipulation depends on the qualifications of the performer.